Erythrasma is a common but often under-recognized skin condition that affects many people worldwide. This article will provide a comprehensive overview of erythrasma, including its symptoms, causes, and treatment options, to help you better understand and manage this condition.
What is Erythrasma?
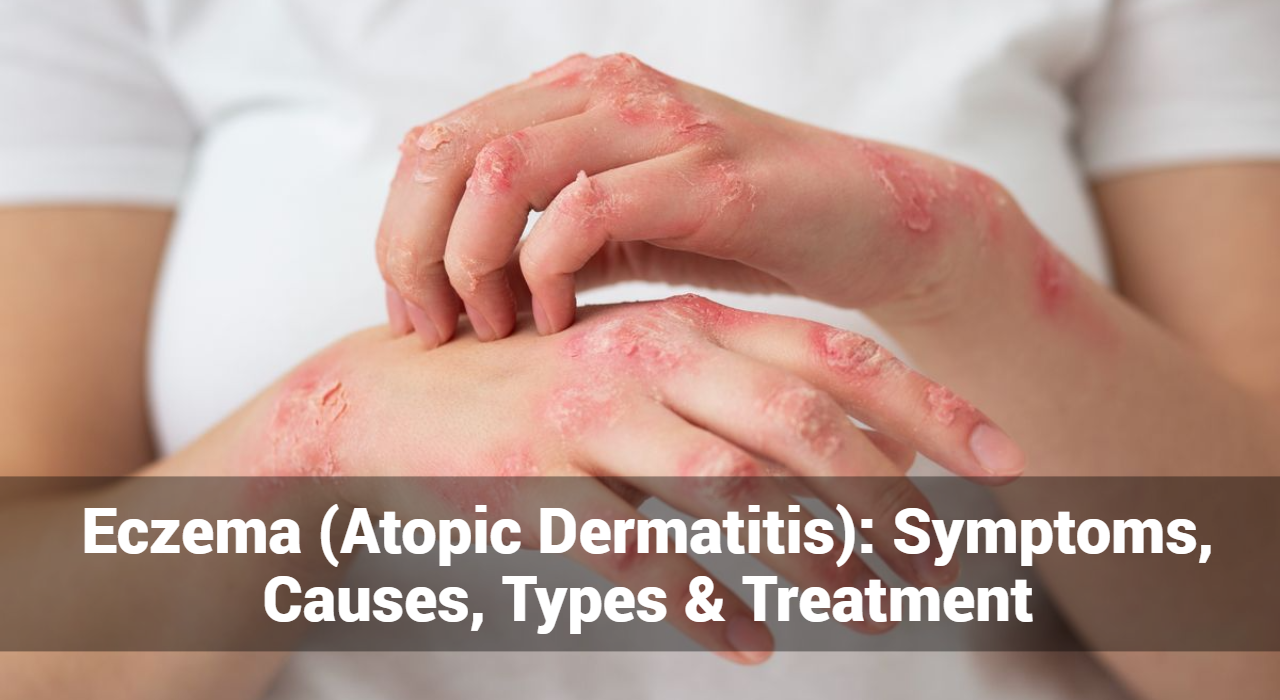
Erythrasma is a chronic skin infection caused by the bacteria Corynebacterium minutissimum. It predominantly affects the skin folds and is characterized by reddish-brown patches with well-defined edges. The condition is often mistaken for other skin disorders, such as fungal infections or eczema, making accurate diagnosis crucial for effective treatment.
Key Characteristics of Erythrasma:
- Color: The lesions often appear as reddish-brown or pinkish-brown patches.
- Location: Commonly affects areas where skin folds, such as the armpits, groin, and under the breasts.
- Appearance: The patches are usually flat, well-defined, and may have a slight scaly texture.
- Symptoms: Itching is generally mild or absent, which helps differentiate it from other similar conditions.
Track and Manage your Eczema treatment using a comprehensive Eczema App
Download Eczemaless now
What Are The Symptoms of Erythrasma?
Erythrasma is characterized by a range of specific symptoms that help in identifying the condition. Here’s a closer look at what to watch for:
- Appearance: The hallmark symptom of erythrasma is the development of reddish-brown or pinkish-brown patches on the skin.
- Edges: These patches are well-defined with clear boundaries, making them easily distinguishable from surrounding skin.
- Skin Folds: Erythrasma predominantly affects areas where skin folds or where there is friction and moisture. Common sites include:
- Armpits (axillae)
- Groin
- Under the breasts (in women)
- Between the toes
- Other Areas: It can occasionally occur in other skin folds or less typical locations.
- Itching: While itching is not a primary feature, some individuals may experience mild itching or discomfort. This is generally less severe compared to other skin conditions.
- Discomfort: A slight burning sensation or tenderness may be present, especially if there is additional irritation or secondary infection.
- Texture: The patches may have a slightly scaly or dry surface, though this is often minimal. The texture can vary, and in some cases, the skin may appear smooth.
- Inflammation: Erythrasma generally does not cause significant inflammation, swelling, or severe redness. The patches are typically stable and do not lead to systemic symptoms.
- Possible Odor: In some cases, especially in warm and humid environments, a mild odor may be noticed. This is due to bacterial activity in moist areas.
What Causes of Erythrasma And Risk Factors?
Erythrasma is caused by an overgrowth of the bacterium Corynebacterium minutissimum. This bacterium is normally present on the skin but can proliferate under certain conditions. Here are the primary causes and risk factors associated with erythrasma:
- Corynebacterium minutissimum: The primary cause of erythrasma is an overgrowth of Corynebacterium minutissimum. This bacterium is part of the normal skin flora but can cause infection when conditions are favorable.
- Warm and Humid Conditions: Erythrasma is more likely to develop in areas where moisture and warmth are prevalent. Skin folds provide an ideal environment for bacterial growth due to trapped heat and sweat.
- Inadequate Cleaning: Insufficient washing or cleansing of skin folds can lead to the accumulation of sweat and bacteria, increasing the risk of erythrasma.
- Diabetes: Individuals with diabetes may be more susceptible to erythrasma due to the impact of high blood sugar levels on skin health.
- Obesity: Excess weight can create additional skin folds and increase moisture, making the skin more prone to bacterial infections.
- Weakened Immune System: A compromised immune system may increase the risk of developing erythrasma as it affects the body’s ability to control bacterial growth.
- Repetitive Friction: Areas subjected to repeated friction, such as from tight clothing, can be more vulnerable to erythrasma. This is especially true in skin folds where friction and moisture can promote bacterial overgrowth.
- Genetic Predisposition: While not a primary cause, some individuals may be genetically predisposed to skin conditions that could make them more susceptible to erythrasma.
- Environmental Factors: Exposure to environmental conditions that promote moisture and heat, such as hot and humid climates, can increase the likelihood of developing erythrasma.
Diagnosis of Erythrasma
Proper diagnosis of erythrasma often involves a combination of clinical evaluation and laboratory tests. Dermatologists typically diagnose erythrasma based on the appearance of the skin lesions and their location. To confirm the diagnosis, a few additional tests may be used:
- Wood’s Lamp Examination: Erythrasma lesions often fluoresce a coral-red color under a Wood’s lamp, which is a handheld UV light.
- Skin Scrapings: In some cases, skin scrapings are examined under a microscope to rule out fungal infections.
- Culture Tests: Culturing a sample from the affected area can help identify Corynebacterium minutissimum.
GET IN CONTROL OF YOUR ECZEMA
Use our AI tool to check the severity of Eczema and keep track of your Eczema progress.
What Are The Treatment Options of Erythrasma?
Treatment of erythrasma typically involves a combination of topical and systemic therapies. The goal is to eliminate the bacteria and alleviate symptoms. Here are the most common treatment options:
1. Topical Antibiotics
Topical antibiotics are often the first line of treatment. They include:
- Erythromycin: Applied directly to the affected areas to combat the bacterial infection.
- Clindamycin: Another effective topical antibiotic that targets Corynebacterium minutissimum.
2. Oral Antibiotics
For more extensive or resistant cases, oral antibiotics may be necessary:
- Doxycycline: A broad-spectrum antibiotic that can effectively treat erythrasma.
- Tetracycline: Another option that may be used for more severe cases.
3. Good Hygiene Practices
Maintaining good hygiene is crucial to prevent recurrence:
- Regular Washing: Clean affected areas thoroughly and regularly with soap and water.
- Drying: Ensure that skin folds are kept dry to inhibit bacterial growth.
- Loose Clothing: Wear breathable, loose-fitting clothing to reduce friction and moisture.
4. Antifungal Treatments
In some cases, antifungal treatments may be used if a fungal infection is also present or suspected:
- Ketoconazole Cream: Used for its antifungal properties to address potential mixed infections.
How Can Prevent Erythrasma?
Preventing erythrasma involves managing risk factors and practicing good hygiene:
- Maintain Dry Skin: Use absorbent powders and wear moisture-wicking clothing to keep skin dry.
- Regular Hygiene: Bathe regularly and thoroughly, especially in areas prone to infection.
- Control Underlying Conditions: Manage diabetes and other conditions that may contribute to skin issues.
When to See a Doctor
While erythrasma is generally not a serious condition, it is important to seek medical advice if:
- You notice persistent or worsening skin lesions.
- Over-the-counter treatments are not effective.
- You have concerns about the diagnosis or management of your skin condition.
Conclusion
Erythrasma is a manageable skin condition when properly diagnosed and treated. Understanding its symptoms, causes, and treatment options can help you effectively address this condition and prevent its recurrence. If you suspect you have erythrasma, consult a dermatologist or healthcare professional for a proper diagnosis and tailored treatment plan. With the right approach, you can alleviate symptoms and maintain healthy skin.
Track and Manage your Eczema treatment using a comprehensive Eczema App
Download Eczemaless now