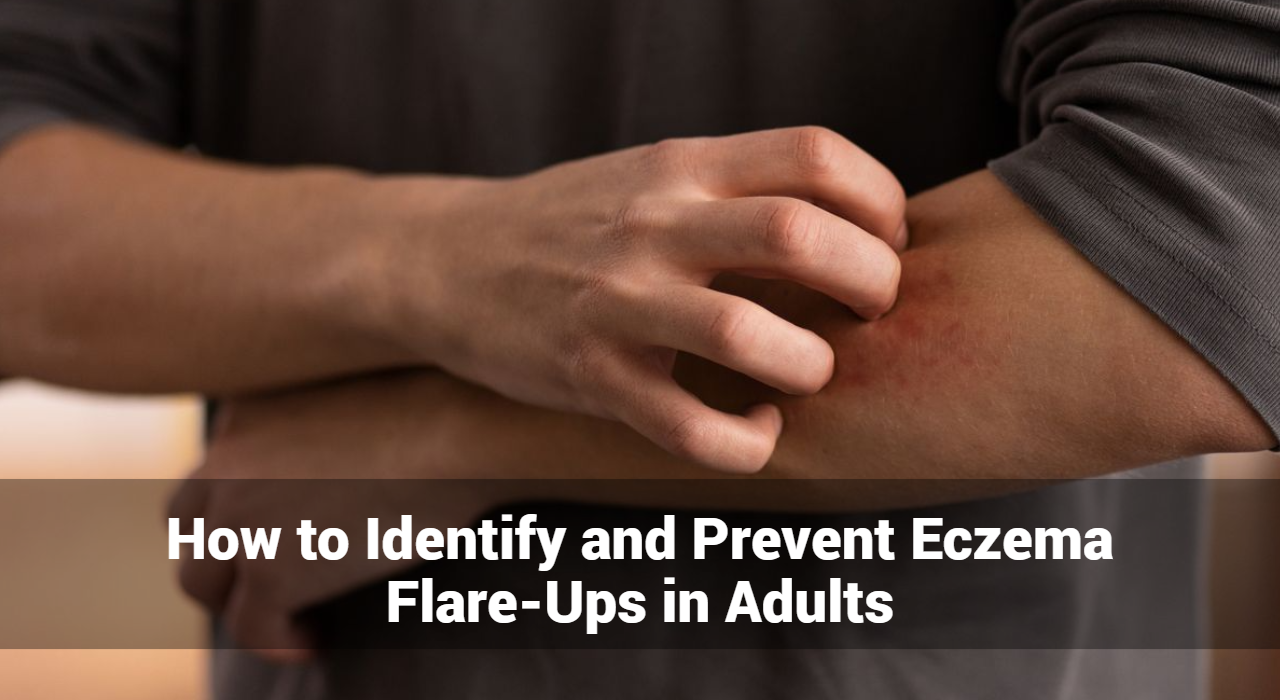
Eczema flare-ups can be a frustrating and uncomfortable experience for adults. Understanding how to identify and prevent these flare-ups is essential for managing the condition effectively. In this article, we will explore the common triggers, symptoms, and preventive measures for eczema flare-ups.
What is Eczema?
Eczema, also known as atopic dermatitis, is a condition that makes the skin red, inflamed, and itchy. It is a common condition that can occur at any age but is more frequently seen in children. Eczema can vary in severity and is often chronic, meaning it can last for a long time, with periods of remission and exacerbation.
What Are Eczema Flare-Ups?
Eczema flare-ups refer to periods when the symptoms of eczema, a chronic skin condition, become significantly worse. These flare-ups are characterized by increased inflammation, itching, redness, and other symptoms that can cause considerable discomfort. Understanding what triggers these flare-ups and how to manage them is essential for individuals living with eczema.
Identifying Eczema Flare-Ups
Eczema flare-ups can be a distressing experience, characterized by a sudden worsening of symptoms. Understanding how to identify these flare-ups is crucial for effective management and timely intervention. In this article, we will delve into the signs, triggers, and strategies for recognizing eczema flare-ups.
Recognizing the Signs of Eczema Flare-Ups
Eczema flare-ups present with a variety of symptoms, often varying in intensity. Here are the key signs to look out for:
- Red, Inflamed Skin
- One of the most noticeable signs of an eczema flare-up is red, swollen patches of skin. These areas may feel warm to the touch and appear puffy.
- Intense Itching
- Itching is a hallmark symptom of eczema. During a flare-up, the itching can become severe, leading to constant scratching that worsens the condition.
- Dry, Scaly Patches
- Flare-ups often cause the skin to become extremely dry and scaly. These patches can be rough and may flake off.
- Blisters and Oozing
- In some cases, small, fluid-filled blisters may form. These blisters can burst, leading to oozing and crusting over.
- Cracked and Painful Skin
- Severely dry skin can crack, creating painful fissures that are susceptible to infection. This can lead to further complications if not treated promptly.
- Thickened Skin
- Chronic scratching and rubbing can cause the skin to thicken and develop a leathery texture, a condition known as lichenification.
Track and Manage your Eczema treatment using a comprehensive Eczema App
Download Eczemaless now
What Are Common Causes of Eczema Flare-Ups in Adults?
Several factors can trigger eczema flare-ups in adults, including:
- Environmental Irritants
- Chemicals: Exposure to harsh chemicals in cleaning products, soaps, and detergents can irritate the skin.
- Pollution: Airborne pollutants can exacerbate eczema symptoms.
- Allergens
- Pollen and Dust: Common allergens like pollen and dust mites can trigger eczema flare-ups.
- Pet Dander: Proteins found in pet dander can cause allergic reactions leading to eczema.
- Weather Conditions
- Cold Weather: Dry, cold air can strip the skin of moisture, leading to flare-ups.
- Hot Weather: Heat and sweat can irritate the skin and cause itching.
- Stress
- Emotional stress can worsen eczema symptoms by triggering the body’s inflammatory response.
- Diet
- Certain foods, such as dairy, nuts, and wheat, can trigger eczema in some individuals.
- Hormonal Changes
- Fluctuations in hormone levels, particularly in women, can lead to eczema flare-ups.
How Can Prevent Eczema Flare-Ups For Adults?
Preventing eczema flare-ups involves a combination of lifestyle adjustments and skincare routines:
- Moisturize Regularly
- Use fragrance-free moisturizers to keep the skin hydrated and prevent dryness. Apply immediately after bathing to lock in moisture.
- Avoid Triggers
- Identify and avoid known triggers, such as specific foods, allergens, and irritants. Keeping a diary can help track what causes flare-ups.
- Manage Stress
- Practice stress-reducing techniques such as yoga, meditation, and deep breathing exercises.
- Wear Protective Clothing
- Use gloves when handling chemicals or cleaning products. Wear loose, breathable clothing to reduce skin irritation.
- Use Gentle Skin Care Products
- Opt for hypoallergenic, fragrance-free soaps, and detergents. Avoid products with harsh chemicals that can irritate the skin.
- Maintain a Healthy Diet
- Eat a balanced diet rich in fruits, vegetables, and omega-3 fatty acids to support skin health.
- Stay Hydrated
- Drink plenty of water to keep your skin hydrated from the inside out.
- Monitor Weather Conditions
- Protect your skin in extreme weather conditions by using a humidifier in dry, cold climates and staying cool in hot weather.
GET IN CONTROL OF YOUR ECZEMA
Use our AI tool to check the severity of Eczema and keep track of your Eczema progress.
Home Remedies for Eczema Flare-Ups in Adults
Managing eczema flare-ups at home can significantly reduce discomfort and improve skin health. While medical treatments are often necessary for severe cases, many individuals find relief through simple, natural remedies. Here are some effective home remedies for managing eczema flare-ups in adults.
1. Moisturize Regularly
Hydration is key to managing eczema. Keeping the skin moisturized helps to prevent dryness and flakiness.
- Use Thick Moisturizers: Opt for thick creams or ointments rather than lotions. Look for products containing ingredients like ceramides, glycerin, or hyaluronic acid.
- Apply After Bathing: Apply moisturizer immediately after bathing to lock in moisture.
2. Warm Baths
Soothing baths can help alleviate itching and inflammation.
- Oatmeal Baths: Adding colloidal oatmeal to a lukewarm bath can soothe the skin and reduce itching. Oatmeal has anti-inflammatory properties that can provide relief.
- Epsom Salt Baths: Epsom salt or Dead Sea salt baths can help reduce inflammation and promote healing.
3. Coconut Oil
Coconut oil has antimicrobial and anti-inflammatory properties.
- How to Use: Apply virgin coconut oil directly to the affected areas to help moisturize and soothe the skin.
4. Aloe Vera
Aloe vera gel is known for its soothing and healing properties.
- How to Use: Apply pure aloe vera gel from the plant or use a store-bought gel with minimal additives. This can help reduce redness and itching.
5. Honey
Honey is a natural antibacterial and anti-inflammatory agent.
- How to Use: Apply raw honey to the affected areas and leave it on for 20-30 minutes before rinsing off. This can help promote healing and reduce flare-ups.
6. Apple Cider Vinegar
Apple cider vinegar can help restore the skin’s natural acidity and fight bacteria.
- How to Use: Dilute apple cider vinegar with equal parts water and apply to the skin using a cotton ball. Rinse off after 5-10 minutes. Be cautious, as it may sting on open or cracked skin.
7. Tea Tree Oil
Tea tree oil has anti-inflammatory and antiseptic properties.
- How to Use: Dilute a few drops of tea tree oil with a carrier oil (like coconut or olive oil) and apply to the affected areas. Avoid using undiluted tea tree oil directly on the skin, as it can cause irritation.
8. Dietary Adjustments
Healthy diet changes can have a positive impact on eczema management.
- Anti-Inflammatory Foods: Include foods rich in omega-3 fatty acids (like fish, flaxseeds, and walnuts), antioxidants (like berries, leafy greens, and nuts), and probiotics (like yogurt and fermented foods).
- Avoid Triggers: Identify and avoid foods that trigger flare-ups. Common triggers include dairy, gluten, and processed foods.
9. Wet Wrap Therapy
Wet wraps can help hydrate and soothe severely dry skin.
- How to Use: After applying moisturizer or medication, cover the affected area with a damp cloth or bandage. Then, cover with a dry layer. Leave on for several hours or overnight.
10. Manage Stress
Stress management techniques can help reduce the frequency and severity of flare-ups.
- Relaxation Techniques: Practice yoga, meditation, deep breathing exercises, or other relaxation techniques to manage stress.
11. Maintain Proper Hygiene
Good hygiene practices can prevent infections and reduce flare-ups.
- Mild Cleansers: Use mild, fragrance-free cleansers that don’t strip the skin of its natural oils.
- Avoid Hot Water: Use lukewarm water for bathing and avoid hot showers, which can dry out the skin.
12. Clothing Choices
Choosing the right clothing can help minimize skin irritation.
- Soft Fabrics: Wear loose-fitting clothes made from soft fabrics like cotton. Avoid scratchy materials like wool.
- Breathable Fabrics: Choose breathable fabrics to reduce sweating and irritation.
Conclusion
By understanding the common triggers and symptoms of eczema flare-ups in adults can take proactive steps to manage their condition and prevent flare-ups. Regular moisturizing, avoiding known triggers, managing stress, and using gentle skincare products are key strategies in maintaining healthy skin. If you continue to experience severe flare-ups, consult a dermatologist for personalized treatment options.
Track and Manage your Eczema treatment using a comprehensive Eczema App
Download Eczemaless now