Table of contents
- Introduction
- Calculating EASI score
- Severity score
- How are the calculations done?
- How do you record the EASI score?
- Severity score X Area score X Multiplier
- What are the advantages of calculating EASI?
- Summary
Introduction
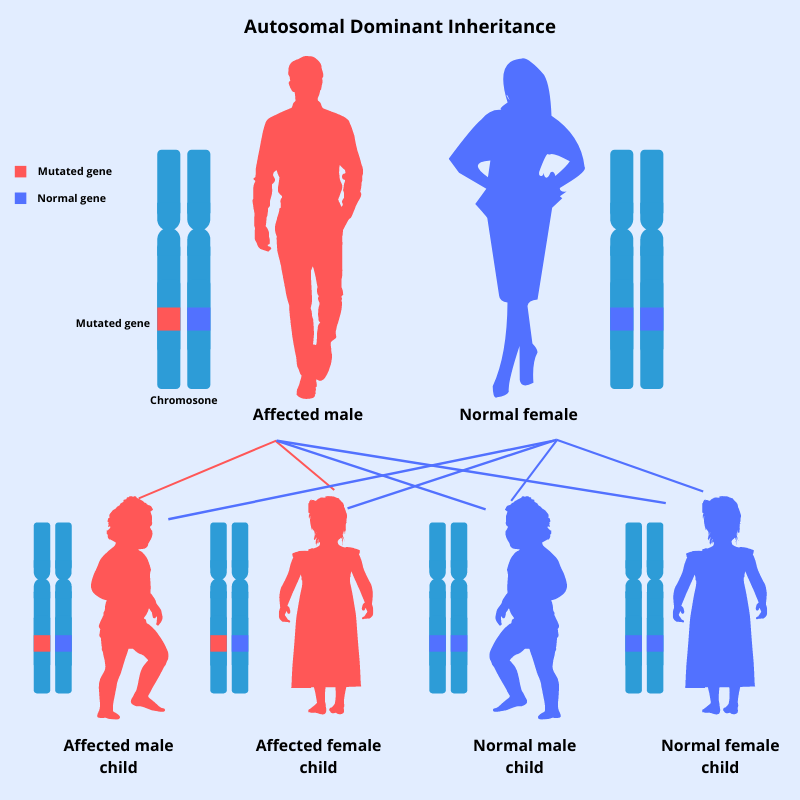
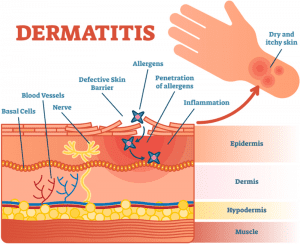
Atopic dermatitis, commonly known as eczema is a common chronic skin condition. Therefore, it is important for doctors or dermatologists to assess its severity and to measure the extent or the area involved in order to manage this condition, as well as to assess the response to treatment in their patients. EASI score is a tool which is used for this purpose. Once you learn how to calculate eczema severity index accurately, it will take only a few minutes to assess an eczema patient. EASI is actually easy!
The Eczema Area and Severity Index (EASI) is a validated scoring system which grades the physical signs of eczema (atopic dermatitis). EASI is a core outcome for measuring the clinical signs of eczema in all clinical trials. However, EASI score includes only the inflamed regions in the body and it does not include a grade for scaling and dryness.
Calculating Eczema Area and Severity Index score
When calculating EASI, 4 body regions are considered. They are;
- Head and neck
- Scalp – 33%
- Face – 17% each side, occupies 33%
- Neck – 17% front and back, occupies 33%
- Trunk including the genital region
- Front – 55%
- Back of trunk – 45%
- Upper limbs
- 50% right arm
- 50% left arm
Front of each arm is 25% and back of each arm is 25%
- Lower limbs including the buttocks
- R/leg – 45%
- L/leg – 45%
Front of each leg is 22.5% and back of each leg is 22.5%
For each of the 4 regions of the body, the area score is recorded. Area score is the total percentage of skin affected with eczema for each body region.
| Area score | Percentage of skin affected by eczema in each region |
| 0 | No active eczema in this region |
| 1 | 1–9% |
| 2 | 10–29% |
| 3 | 30–49% |
| 4 | 50–69% |
| 5 | 70–89% |
| 6 | 90–100%: the entire region is affected by eczema |
Track and Manage your Eczema treatment using a comprehensive Eczema App
Download Eczemaless now
Severity score
The severity score is also recorded for each region of the body. It is calculated as the sum of the intensity score using 4 different signs. These 4 signs include;
- Scratching and excoriation
- Redness of skin (erythema and inflammation)
- Thickness of skin (swelling and induration in acute eczema)
- Lichenification (lined skin with furrows and prurigo nodules in chronic eczema.
Half scores are permitted. It is difficult to assess redness in patients with a dark complexion. Therefore, if you are in doubt, you can increase the average redness score by 1 level.
| Score | Intensity of redness, thickness/swelling, scratching, lichenification |
| 0 | None, absent |
| 1 | Mild (just perceptible) |
| 2 | Moderate (obvious) |
| 3 | Severe |
How are the calculations done?
You have to record the intensity of each 4 signs for all 4 regions separately and calculate the severity score.
- Severity score = scratching intensity + thickness intensity + redness intensity + lichenification intensity
For each region, multiple the area score by the severity score and by a multiplier. Note that the multiplier is different for each of the body region and is also different in children.
- Head and neck: severity score x area score x 0.1 (in children from 0–7 years the multiplier is 0.2)
- Trunk: severity score x area score x 0.3
- Upper limbs: severity score x area score x 0.2
- Lower limbs: severity score x area score x 0.4 (in children from 0–7 years the multiplier is 0.3)
To determine the final EASI score, add up the total scores for each region. The minimum EASI score is 0. The maximum EASI score will be 72.
How do you record the EASI score?
| Body region | Redness | Thickness | Scratching | Lichenification | Severity score | Area score | Multiplier | Region score |
| Head/neck | _______ | +_______ | +_______ | +_______ | =_______ | X_______ | X 0.1 (If ≤7 yrs, X 0.2) | =_______ |
| Trunk | _______ | +_______ | +_______ | +_______ | =_______ | X_______ | X 0.3 | =_______ |
| Upper limbs | _______ | +_______ | +_______ | +_______ | =_______ | X_______ | X 0.2 | =_______ |
| Lower limbs | _______ | +_______ | +_______ | +_______ | =_______ | X_______ | X 0.4 (If ≤7 yrs, X 0.3) | =_______ |
| The final EASI score: add up the 4 region scores | =_______ (0-72) | |||||||
All regions has to be added up separately to get each region score. Then the values of each region score in all 4 regions must be added together. Then you will be able to calculate the final EASI score which will be between 0-72.
To help you understand better, let us look at an example of a child with an acute flare of eczema and calculate the EASI score.
Ex: A 5 year old girl has developed an acute flare up of eczema. This flare up has affected all her limb flexures. The trunk of this child is reddish and dry.
Now let us calculate the region scores.
- Since the head and neck is not affected, the score in this region is zero. (severity score = 0 and area score is also 0)
- The trunk is mildly red which gets 1 point. Since it is not scratched and not lichenified no points are given. Skin is thickened only mildly, therefore, can give 1 point. When the points are added thee severity score is 2.
The trunk is affected around 60%, therefore the area score is 4.
- Skin in both elbow flexures are affected by eczema and it is moderately red (2), moderately scratched (2), only mildly thickened (1) but since it is not lichenified it is 0. The severity score adds to 8.
Area score is 1 because less than 10% of both upper limbs are affected.
- Eczema behind both knees are extremely red and is quite severe. 3 points are given. They are severely scratched (3), with severe thickening (3) and mild lichenification (1) is seen. Therefore thee severity score is 10.
Area score is 2, because around 20% of the legs are affected.
Now let us calculate the region score for each of the regions.
Severity score X Area score X Multiplier
- Head and neck = 0
- Trunk = 2 x 4 x 0.3 = 2.4
- Upper limbs = 5 x 1 x 0.2 = 1
- Lower limbs = 10 x 2 x 0.3 = 6.0
EASI score = 2.4 + 1.0 + 6.0 = 9.4
The 5 year old girl with an acute flare of eczema was found to have an EASI score of 9.4.
What are the advantages of calculating EASI?
EASI (Eczema Area and Severity Index ) is a tool or a scale used in clinical trials to assess the extent and severity of eczema. The highest score is 72 which indicates worse severity of eczema. It has been suggested that severity of eczema based on EASI score can be categorized as follows;
- 0 = Clear
- 1 – 1.0 = Almost clear
- 1 – 7 = Mild atopic dermatitis
- 1 – 21 = Moderate severity of atopic dermatitis
- 1 – 50 = Severe atopic dermatitis
- 1 – 72 = Very severe atopic dermatitis
In the example stated above, the 5 year old girl who had an acute flare of eczema falls to the category of moderate severity.
EASI score can also be used to assess the response to treatment.
Summary
The Eczema Area and Severity Index (EASI) is a validated scoring system which grades the physical signs of eczema. The body is divided in to 4 regions and the calculation is done by adding up scores of each region.
EASI score = Severity score X Area score X Multiplier
The severity and extent of eczema can be assessed by calculating thee EASI score and it is an important tool used in clinical trials.
References:
https://dermnetnz.org/topics/easi-score
https://journals.sagepub.com/doi/10.1177/1203475420923644
https://www.ncbi.nlm.nih.gov/books/NBK539234/
GET IN CONTROL OF YOUR ECZEMA
Use our AI tool to check the severity of Eczema and keep track of your Eczema progress.