In the intricate landscape of pediatric dermatology, the skin of children demands specialized attention and care. From infancy to adolescence, the delicate nature of pediatric skin presents unique challenges and considerations for parents and caregivers. Understanding the fundamentals of pediatric dermatology is paramount in ensuring the health and well-being of our youngest generation.
Introduction to Pediatric Dermatology
Pediatric dermatology encompasses the diagnosis, treatment, and management of skin conditions in infants, children, and adolescents. Unlike adult skin, which has reached maturity, children’s skin is still developing, rendering it more susceptible to certain disorders and infections. Additionally, children may not always communicate their discomfort effectively, underscoring the importance of vigilance and proactive care.
Common Skin Conditions in Children
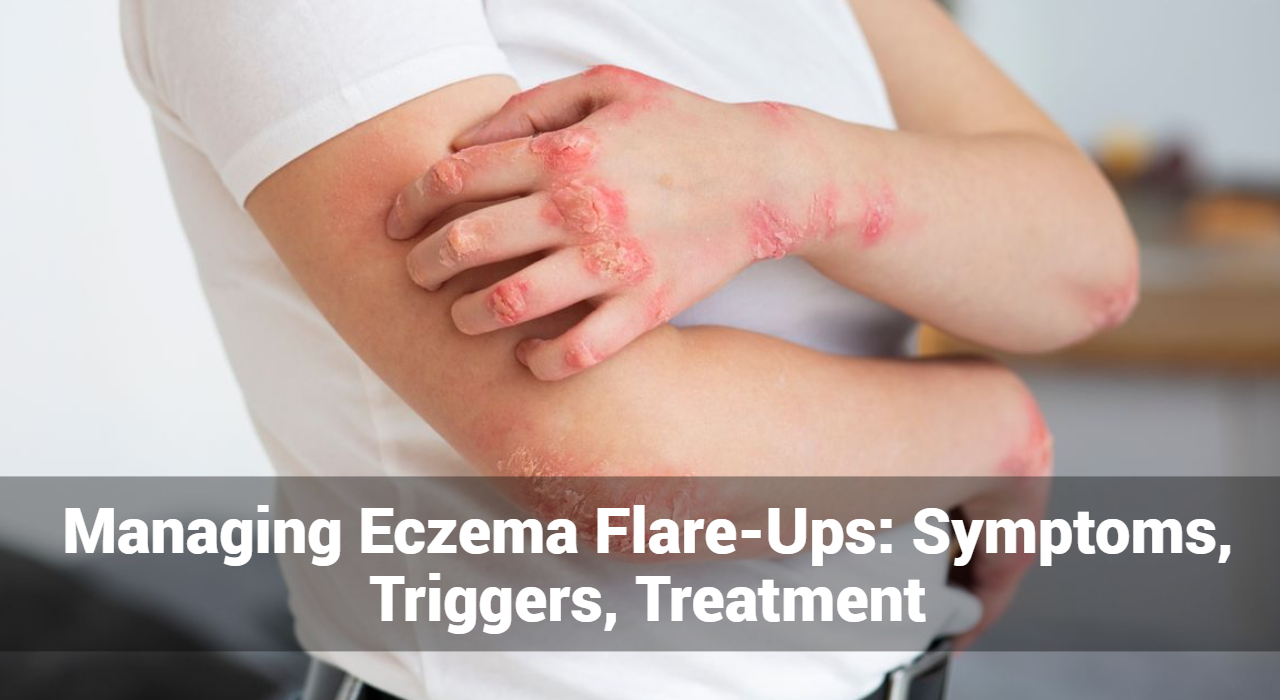
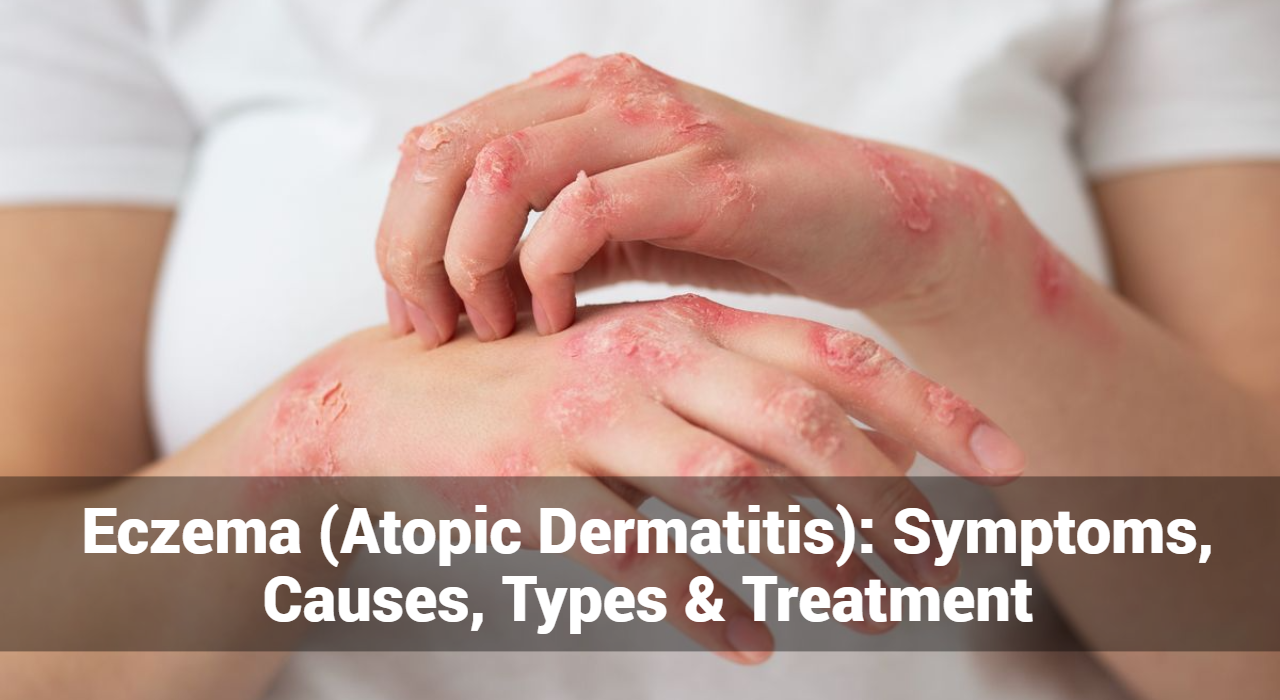
- Eczema (Atopic Dermatitis): Eczema ranks among the most prevalent skin conditions in children, characterized by dry, itchy, and inflamed skin. It frequently manifests on the face, elbows, and knees, impacting a child’s comfort and quality of life.
- Diaper Dermatitis: Diaper rash, or diaper dermatitis, arises from prolonged exposure to moisture, urine, and feces in diapers. It presents as redness, irritation, and discomfort in the diaper area, necessitating gentle care and frequent diaper changes.
- Acne: Although commonly associated with adolescence, acne can emerge in children as young as 8 or 9 years old. Managing childhood acne involves gentle cleansing, avoidance of harsh products, and, in some cases, consultation with a dermatologist for specialized treatment.
- Birthmarks: Birthmarks are commonplace in newborns and can be either vascular (e.g., hemangiomas) or pigmented (e.g., moles). While most birthmarks are benign, some may warrant monitoring or intervention, especially if they pose cosmetic or medical concerns.
Developmental Aspects of Pediatric Skin
Children’s skin undergoes significant developmental changes from birth through adolescence. At birth, a newborn’s skin is delicate and vulnerable, gradually developing in thickness, texture, and resilience over time. Factors such as hormonal changes, environmental exposures, and genetic predispositions influence the development and function of pediatric skin.
Diagnosis and Treatment Approaches
Diagnosing skin conditions in children requires a thorough evaluation, often involving a combination of medical history, physical examination, and diagnostic tests. Treatment approaches may vary depending on the specific condition, its severity, and the child’s age and medical history. Common treatment modalities include topical medications, oral medications, phototherapy, and procedural interventions.
Essential Tips for Pediatric Skin Care
- Gentle Cleansing: Choose mild, fragrance-free cleansers and moisturizers specifically formulated for children’s sensitive skin. Avoid products containing harsh chemicals or allergens that may exacerbate skin conditions.
- Sun Protection: Shield your child’s skin from harmful ultraviolet (UV) rays by applying sunscreen with a sun protection factor (SPF) of at least 30. Encourage the use of hats, sunglasses, and protective clothing, particularly during outdoor activities.
- Hydration: Ensure your child remains adequately hydrated by encouraging them to drink plenty of water throughout the day. Proper hydration supports skin health and helps prevent dryness and irritation.
- Healthy Diet: Emphasize a balanced diet rich in fruits, vegetables, whole grains, and lean proteins, as nutrition plays a vital role in skin health. Limit sugary snacks and processed foods, which can contribute to inflammation and exacerbate certain skin conditions.
- Promote Good Hygiene: Teach children the importance of proper hygiene practices, including regular handwashing with mild soap and water. Encourage them to avoid scratching or picking at their skin, as this can worsen existing skin conditions or lead to infections.
- Regular Check-ups: Schedule routine visits with a pediatrician or dermatologist to monitor your child’s skin health and address any concerns promptly. Early detection and intervention are key to preventing complications and promoting optimal skin wellness.
Track and Manage your Eczema treatment using a comprehensive Eczema App
Download Eczemaless now
Navigating Pediatric Dermatology: A Holistic Approach
In addition to addressing specific skin conditions, pediatric dermatology encompasses a holistic approach to children’s skin health and well-being. This includes considering factors such as:
- Environmental Influences: Recognizing the impact of environmental factors, such as pollution, climate, and allergens, on children’s skin health. Taking steps to minimize exposure to potential irritants and allergens can help maintain a healthy skin barrier.
- Psychosocial Factors: Acknowledging the psychosocial impact of skin conditions on children, including feelings of self-consciousness, anxiety, and low self-esteem. Providing emotional support and fostering open communication can empower children to cope with their condition and thrive socially and emotionally.
- Family History: Understanding the role of genetics in certain skin conditions, such as eczema, psoriasis, and melanoma. A family history of skin disorders may increase a child’s risk, warranting closer monitoring and proactive management.
- Individualized Care: Recognizing that every child is unique and may respond differently to treatment approaches. Tailoring care plans to meet the specific needs and preferences of each child ensures the best possible outcomes.
The Role of Pediatric Dermatologists
Pediatric dermatologists play a pivotal role in the comprehensive care of children with skin conditions. These specialized healthcare providers possess expertise in diagnosing and treating a wide range of pediatric dermatological disorders, from common concerns to rare genetic conditions.
Key responsibilities of pediatric dermatologists include:
- Diagnostic Evaluation: Conducting thorough evaluations to accurately diagnose skin conditions in children, taking into account their age, medical history, and clinical presentation. This may involve performing skin biopsies, allergy testing, or other diagnostic procedures as needed.
- Treatment Planning: Developing individualized treatment plans tailored to each child’s specific condition, severity, and unique needs. Treatment modalities may include topical medications, oral medications, phototherapy, or procedural interventions, depending on the diagnosis.
- Education and Counseling: Providing education and guidance to parents and caregivers on proper skin care techniques, lifestyle modifications, and strategies for managing their child’s condition effectively. Empowering families with knowledge equips them to play an active role in their child’s skin health.
- Collaborative Care: Collaborating with other healthcare professionals, including pediatricians, allergists, immunologists, and psychologists, to deliver comprehensive, multidisciplinary care. This team-based approach ensures that all aspects of the child’s health and well-being are addressed.
Preventive Measures and Home Care Tips
Preventive measures and proper home care play a crucial role in maintaining children’s skin health. Key tips for pediatric skin care include:
- Gentle cleansing with mild, fragrance-free products
- Regular moisturization to prevent dryness and irritation
- Avoidance of harsh chemicals and allergens
- Sun protection with sunscreen, protective clothing, and shade
- Promotion of good hygiene practices, such as handwashing and nail trimming
By incorporating these practices into daily routines, parents and caregivers can help prevent skin problems and promote overall skin wellness in children.
Importance of Sun Protection
Sun protection is particularly important in pediatric dermatology, as childhood sun exposure can have long-lasting effects on skin health. Ultraviolet (UV) radiation from the sun can cause sunburn, premature aging, and increase the risk of skin cancer later in life. Therefore, it is crucial to protect children’s skin from the sun’s harmful rays by:
- Applying sunscreen with a sun protection factor (SPF) of at least 30
- Reapplying sunscreen every two hours, or more frequently if swimming or sweating
- Seeking shade during peak sun hours (10 a.m. to 4 p.m.)
- Dressing children in protective clothing, hats, and sunglasses
- Avoiding tanning beds and other sources of artificial UV radiation
By instilling sun-safe habits early in life, parents can help reduce their children’s risk of sun-related skin damage and promote lifelong sun protection practices.
Emotional and Psychosocial Impact
Skin conditions can have a significant emotional and psychosocial impact on children, affecting their self-esteem, social interactions, and overall quality of life. Children with visible skin disorders may experience feelings of embarrassment, shame, or anxiety, leading to social withdrawal and decreased participation in activities. It is essential for parents, caregivers, and healthcare providers to address not only the physical symptoms of skin conditions but also the emotional and psychological needs of affected children.
Pediatric Dermatology: A Multidisciplinary Approach
Pediatric dermatology often involves a multidisciplinary approach, with collaboration among dermatologists, pediatricians, allergists, immunologists, psychologists, and other healthcare professionals. This team-based approach allows for comprehensive evaluation, treatment, and management of pediatric skin conditions, addressing both medical and psychosocial aspects of care. By working together, healthcare providers can ensure that children receive holistic, individualized care that meets their unique needs and promotes optimal health and well-being.
Parental Education and Support
Parents play a crucial role in managing their children’s skin conditions, from implementing preventive measures to following treatment plans and providing emotional support. Parental education is essential in pediatric dermatology, empowering parents with the knowledge and skills needed to care for their children’s skin effectively. Healthcare providers should provide clear, concise information about skin conditions, treatment options, and home care strategies, as well as offer ongoing support and guidance to parents throughout the treatment process.
Conclusion
Pediatric dermatology encompasses a multifaceted approach to caring for the skin health of children, addressing both common concerns and complex conditions with sensitivity and expertise. By prioritizing gentle care, sun protection, hydration, and regular monitoring, parents and caregivers can help safeguard their little ones’ skin and promote lifelong wellness.
Through collaboration with pediatric dermatologists and a commitment to holistic care, children can navigate skin conditions with confidence and resilience, allowing them to thrive and embrace the world around them. By investing in the health of our youngest generation’s skin, we lay the foundation for a lifetime of healthy habits and radiant skin.