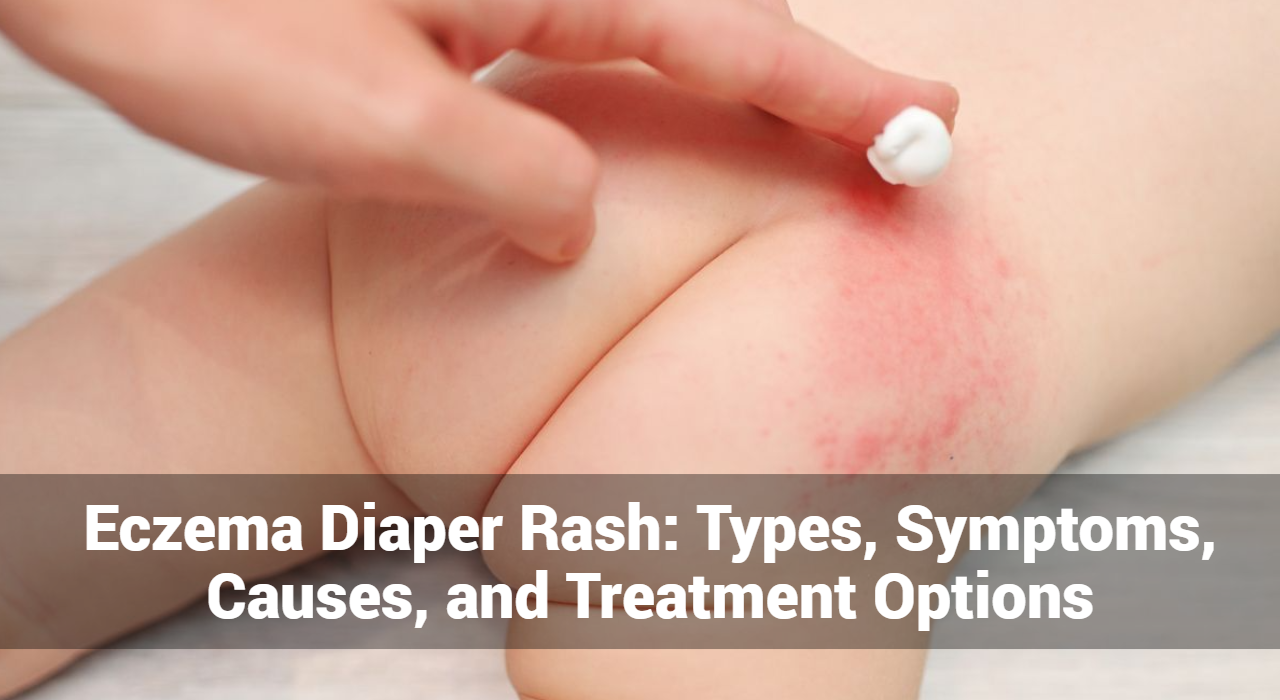
Eczema diaper rash, also known as diaper dermatitis, is a common condition characterized by inflamed, irritated skin in the diaper area. While diaper rash is often associated with contact irritation or moisture, it can also be exacerbated by eczema, a chronic inflammatory skin condition. Understanding the types, symptoms, causes, and treatment options for eczema diaper rash is crucial for effective management and relief for infants and toddlers.
What Are They Types of Eczema Diaper Rash?
Eczema diaper rash encompasses various types of diaper dermatitis that are influenced by underlying eczema or atopic dermatitis. While diaper rash itself can have multiple causes, eczema diaper rash specifically refers to diaper dermatitis that is exacerbated by eczema or atopic dermatitis. Here are the types of eczema diaper rash:
- Contact Dermatitis:
- Contact dermatitis is a type of eczema diaper rash caused by irritation or allergic reactions to substances that come into contact with the skin in the diaper area. These substances may include urine, feces, diapers, wipes, detergents, or chemicals.
- Atopic Dermatitis (Eczema) in the Diaper Area:
- Atopic dermatitis, commonly known as eczema, can affect the diaper area in infants and young children. This type of eczema diaper rash is characterized by red, inflamed, itchy patches of skin in the diaper region. It may be associated with other symptoms of eczema, such as dryness, scaling, or oozing.
- Seborrheic Dermatitis:
- Seborrheic dermatitis is a common condition characterized by red, greasy, scaly patches of skin, often occurring on the scalp, face, and diaper area. While it is not typically considered a primary type of eczema, seborrheic dermatitis can contribute to eczema diaper rash, particularly in infants.
- Irritant Contact Dermatitis:
- Irritant contact dermatitis is a non-allergic type of eczema diaper rash caused by exposure to irritants such as urine, feces, friction, or harsh chemicals in diapers, wipes, or detergents. It leads to redness, inflammation, and sometimes blistering or peeling of the skin.
- Allergic Contact Dermatitis:
- Allergic contact dermatitis occurs when the skin in the diaper area comes into contact with allergens, triggering an immune response and causing eczema-like symptoms. Common allergens include fragrances, preservatives, latex, metals (e.g., nickel), or certain chemicals in diapers or wipes.
- Yeast or Fungal Diaper Rash:
- While not directly related to eczema, yeast or fungal diaper rash can exacerbate eczema symptoms in the diaper area. Candida albicans, a type of yeast, thrives in warm, moist environments, leading to red, inflamed, and sometimes pustular lesions in the diaper region.
These types of eczema diaper rash can overlap or coexist, making diagnosis and management challenging. Proper identification of the underlying causes and triggers is essential for effective treatment and prevention of eczema diaper rash. If you suspect your child has eczema diaper rash or if the rash persists despite home remedies, consult a healthcare professional for evaluation and personalized treatment recommendations.
Track and Manage your Eczema treatment using a comprehensive Eczema App
Download Eczemaless now
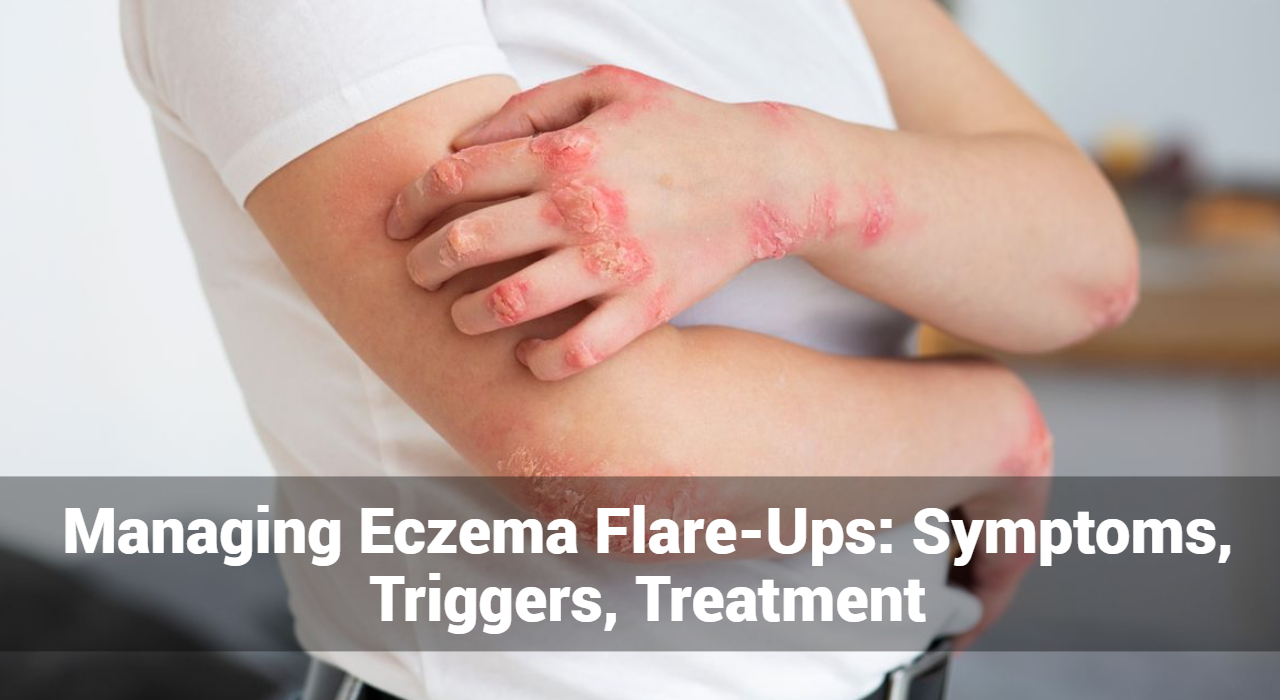
What Are The Common Symptoms of Diaper Rash?
Eczema diaper rash shares symptoms with both traditional diaper rash and eczema, presenting as a combination of skin irritation and inflammation in the diaper area. Here are the common symptoms of eczema diaper rash:
- Redness and Inflammation: The affected skin in the diaper area may appear red, irritated, and inflamed. This redness can vary in intensity and may extend beyond the area covered by the diaper.
- Itching: Itching is a hallmark symptom of eczema and may be pronounced in eczema diaper rash. Infants may exhibit signs of discomfort, such as fussiness or increased crying, due to persistent itching.
- Dry, Flaky Skin: The skin affected by eczema diaper rash may appear dry, rough, or flaky. This dryness can contribute to further irritation and discomfort for the infant.
- Raised Bumps or Patches: Raised bumps or patches of skin may develop in the diaper area, contributing to the overall inflammation and discomfort experienced by the infant.
- Oozing or Crusting: In severe cases, eczema diaper rash may lead to oozing or crusting of the affected skin. This occurs when the skin becomes inflamed and damaged, leading to the release of fluid or the formation of crusts.
- Blisters: In some instances, eczema diaper rash may manifest as fluid-filled blisters on the skin. These blisters can be painful and may rupture, leading to further irritation and potential infection.
- Thickened or Lichenified Skin: Prolonged or chronic eczema diaper rash can result in thickened, leathery skin in the diaper area. This condition, known as lichenification, occurs due to repeated scratching and rubbing of the affected skin.
- Secondary Infections: Eczema diaper rash increases the risk of secondary bacterial or fungal infections due to the compromised skin barrier. Signs of infection may include warmth, tenderness, swelling, or the presence of pus-filled lesions.
- Discomfort during Diaper Changes: Infants with eczema diaper rash may exhibit discomfort or agitation during diaper changes due to the sensitivity and inflammation of the affected skin.
- Chronic or Recurrent Rash: Eczema diaper rash tends to be chronic or recurrent, with periods of flare-ups followed by periods of remission. Despite treatment, the rash may persist or recur, requiring ongoing management and care.
If your infant exhibits any of these symptoms of eczema diaper rash, it’s essential to seek medical advice for proper evaluation and treatment. A healthcare professional, such as a pediatrician or dermatologist, can provide personalized recommendations to alleviate symptoms and manage the condition effectively.
Causes of Eczema Diaper Rash:
Eczema diaper rash, also known as diaper dermatitis with an eczematous component, can be triggered by various factors that contribute to skin irritation and inflammation in the diaper area. Understanding the causes of eczema diaper rash is essential for effective management and prevention. Here are common causes:
- Contact Irritants: Exposure to irritants such as urine, feces, or chemicals in diapers, wipes, detergents, or baby products can irritate the delicate skin in the diaper area. Prolonged contact with wet or soiled diapers can weaken the skin barrier and increase susceptibility to irritation.
- Friction: Rubbing or chafing of the skin against diapers, clothing, or bedding can exacerbate skin irritation and contribute to the development of eczema diaper rash. Tight-fitting diapers or clothing may increase friction and aggravate the condition.
- Moisture: Prolonged exposure to moisture from urine, sweat, or inadequate drying after bathing can weaken the skin barrier and promote skin irritation and inflammation. Moist environments create an ideal breeding ground for bacteria and fungi, further exacerbating the rash.
- Microbial Factors: Overgrowth of yeast (Candida albicans) or bacteria in the diaper area can contribute to diaper rash development. Warm, moist environments, such as those created by wet diapers, provide optimal conditions for microbial growth and colonization.
- Skin Sensitivities: Infants with atopic dermatitis (eczema) or sensitive skin may be more prone to developing eczema diaper rash due to their skin’s heightened reactivity to irritants and allergens. Genetic factors, immune system dysfunction, and environmental triggers can contribute to skin sensitivities.
- Allergic Reactions: Allergic reactions to ingredients in diapers, wipes, laundry detergents, or baby products can trigger eczema diaper rash in susceptible individuals. Common allergens include fragrances, dyes, preservatives, latex, or chemicals used in diaper manufacturing.
- Dietary Factors: Certain foods or ingredients in breast milk or formula may contribute to diaper rash in breastfed or formula-fed infants. Cow’s milk protein, soy, eggs, and citrus fruits are common dietary triggers for allergic reactions that can manifest as eczema diaper rash.
- Environmental Factors: Environmental allergens such as pollen, dust mites, pet dander, or mold spores can exacerbate eczema symptoms in the diaper area. Exposure to these allergens through contact or inhalation can trigger allergic reactions and contribute to rash development.
- Heat and Sweat: Excessive heat and sweating in the diaper area can exacerbate skin irritation and promote rash development. Hot and humid weather conditions or overdressing can increase sweating and worsen eczema symptoms.
- Underlying Skin Conditions: Pre-existing skin conditions such as atopic dermatitis (eczema), seborrheic dermatitis, psoriasis, or irritant or allergic contact dermatitis can predispose infants to eczema diaper rash. These conditions may disrupt the skin barrier and increase susceptibility to irritation and inflammation.
By identifying and addressing the underlying causes of eczema diaper rash, parents and caregivers can take proactive steps to prevent flare-ups and promote healthy skin in the diaper area. If eczema diaper rash persists or worsens despite home remedies, consult a healthcare professional for evaluation and personalized treatment recommendations.
GET IN CONTROL OF YOUR ECZEMA
Use our AI tool to check the severity of Eczema and keep track of your Eczema progress.
Treatment Options for Eczema Diaper Rash:
- Frequent Diaper Changes: Change diapers promptly whenever they become wet or soiled to minimize skin exposure to moisture and irritants.
- Gentle Cleansing: Use mild, fragrance-free baby wipes or plain water to clean the diaper area during diaper changes. Avoid harsh soaps, alcohol-based wipes, or wipes containing potential irritants.
- Pat Dry: Gently pat the skin dry with a soft cloth or allow it to air dry completely before applying a diaper cream or ointment.
- Barrier Creams: Apply a thick layer of barrier cream or ointment containing zinc oxide or petroleum jelly to protect the skin and create a barrier against moisture and irritants.
- Topical Steroids: In cases of severe inflammation or eczema flare-ups, a healthcare provider may prescribe a mild topical corticosteroid cream or ointment to reduce inflammation and itching. Use as directed and under medical supervision.
- Moisturizers: Apply a gentle, fragrance-free moisturizer to the diaper area regularly to keep the skin hydrated and maintain its natural barrier function.
- Antifungal Creams: If a yeast infection is suspected, an antifungal cream or ointment may be prescribed to treat the underlying fungal overgrowth.
- Oral Antihistamines: In some cases, oral antihistamines may be recommended to help alleviate itching and discomfort associated with eczema diaper rash. Consult a healthcare provider for appropriate dosage and recommendations.
- Avoidance of Triggers: Identify and avoid potential triggers that exacerbate eczema diaper rash, such as certain foods, fabrics, or environmental allergens.
- Consultation with Healthcare Provider: If eczema diaper rash persists, worsens, or is accompanied by signs of infection (e.g., fever, pus-filled blisters), seek medical advice from a pediatrician or dermatologist for further evaluation and treatment recommendations.
In conclusion
Eczema diaper rash can be a challenging condition to manage, but with proper care, most cases can be effectively treated and prevented. By understanding the types, symptoms, causes, and treatment options for eczema diaper rash, parents and caregivers can take proactive steps to promote healthy skin and provide relief for their little ones. If you have concerns about your child’s diaper rash, don’t hesitate to consult a healthcare professional for personalized advice and guidance.