Eczema is a challenging condition that affects millions of people worldwide, causing discomfort, itching, and inflammation. Managing eczema effectively requires a combination of personalized care, accurate information, and consistent tracking. The Eczemaless App is a cutting-edge tool designed to revolutionize eczema care. Here are five compelling reasons to use the Eczemaless App for your eczema care today:
1. Personalized Eczema Management Plans
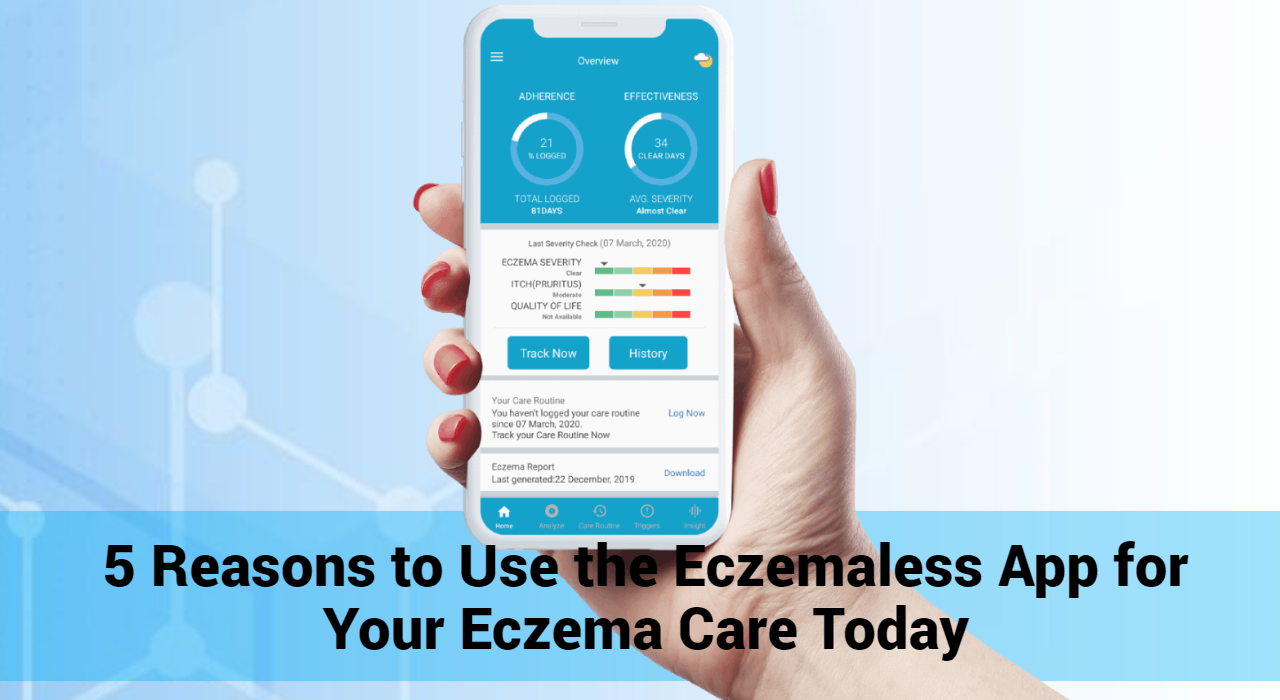
The Eczemaless App provides personalized management plans tailored to your specific needs. When you first use the app, it asks detailed questions about your eczema symptoms, triggers, and treatment history. Using this information, the app creates a customized care plan that includes recommendations for skincare routines, dietary adjustments, and environmental modifications. Personalized plans ensure that you are using the most effective strategies to manage your eczema, reducing flare-ups, and improving your quality of life.
2. Determine If Your Treatments Are Working by Regularly Tracking Symptoms and Triggers
- Detailed Symptom and Trigger Logs: The Eczemaless App allows you to keep comprehensive logs of your symptoms, triggers, and treatment responses. This detailed record provides your doctor with a clear and thorough picture of your condition over time. By sharing these logs during appointments, you can have more informed and productive discussions about your treatment plan.
- Visual Progress Reports: The app generates visual reports, such as graphs and charts, that illustrate your symptoms and treatment progress. These visual aids can help both you and your doctor quickly identify trends and patterns. With this information, you can engage in more meaningful conversations about what is and isn’t working in your treatment plan.
- Personalized Treatment Feedback: With the Eczemaless App, you can provide real-time feedback on how well your treatments are working. This ongoing dialogue allows your doctor to make timely adjustments to your treatment plan, ensuring it remains effective and tailored to your needs. By actively participating in the evaluation process, you can help your doctor understand your unique response to different therapies.
- Preparation for Appointments: Using the app to prepare for your appointments can make your consultations more efficient and productive. By reviewing your symptom logs, triggers, and treatment responses ahead of time, you can identify key points you want to discuss with your doctor. This preparation helps ensure that all important issues are addressed during your visit.
- Shared Decision-Making Tools: The Eczemaless App supports shared decision-making by providing educational resources and tools that help you understand your condition and treatment options. With this knowledge, you can engage in more informed discussions with your doctor, ask relevant questions, and collaborate on decisions that best suit your health needs and lifestyle.
- Real-Time Communication Features: Some versions of the Eczemaless App may offer real-time communication features, such as messaging or video calls, allowing you to stay in touch with your doctor between appointments. This continuous communication ensures that you can address any concerns or changes in your condition promptly, leading to better overall management of your eczema.
- Tracking and Monitoring Treatment Outcomes: By regularly tracking and monitoring your treatment outcomes using the app, you can provide your doctor with accurate and up-to-date information. This data-driven approach helps your doctor make evidence-based decisions about your care, leading to more effective and personalized treatment plans.
- Educational Resources and Support: The Eczemaless App offers access to a wealth of educational resources, including articles, videos, and expert advice. By staying informed about your condition, you can engage in more meaningful conversations with your doctor and make well-informed decisions about your care.
4. Real-Time Progress Monitoring Using the Eczemaless App
Monitoring your progress is crucial for effective eczema management. The Eczemaless App features real-time progress tracking, allowing you to see how your symptoms evolve over time. The app generates visual graphs and charts based on your symptom logs, giving you a clear picture of your eczema’s progression. This feature not only helps you stay motivated by showing improvements but also enables you to make data-driven decisions about your treatment plan. Real-time monitoring ensures you can adjust your strategies promptly and effectively.
GET IN CONTROL OF YOUR ECZEMA
Use our AI tool to check the severity of Eczema and keep track of your Eczema progress.
5. Help Inform Advances in Eczema Research by Using the Eczemaless App
Managing skin conditions effectively involves not only personalized care but also contributing to the broader understanding of eczema through research. The Eczemaless App is a powerful tool designed to aid individuals in managing their eczema while simultaneously advancing eczema research. Here’s how using the Eczemaless App can help inform advances in eczema research:
- Comprehensive Data Collection
The Eczemaless App collects detailed data about your eczema symptoms, triggers, treatment responses, and daily habits. This comprehensive data set provides valuable insights into the patterns and factors influencing eczema, helping researchers identify common trends and potential new treatments.
- Real-Time Symptom Tracking
By regularly logging your symptoms in the app, you create a rich database of real-time information. Researchers can use this data to analyze the effectiveness of different treatments over time, improving their understanding of how eczema progresses and responds to various interventions.
- Identifying Triggers and Patterns
The app’s ability to track potential triggers, such as food, stress, weather, and environmental factors, helps researchers identify common triggers and their impact on eczema flare-ups. This information is crucial for developing targeted strategies to prevent and manage eczema.
- Anonymous Data Sharing
The Eczemaless App allows users to share their data anonymously with researchers. This ensures your privacy while contributing valuable information to scientific studies. The aggregated data from many users can lead to significant breakthroughs in understanding eczema and developing new treatments.
- Feedback on Treatment Effectiveness
The app’s symptom tracking and progress monitoring features provide real-time feedback on treatment effectiveness. Researchers can use this information to evaluate the efficacy of existing treatments and explore new therapeutic options, ultimately improving care for eczema patients.
- Patient-Reported Outcomes
Patient-reported outcomes are vital for understanding the real-world impact of eczema and its treatments. By using the Eczemaless App, you contribute firsthand information about your experiences, helping researchers develop more patient-centered approaches and improve quality of life for those with eczema.
- Participating in Clinical Studies
The Eczemaless App may offer opportunities to participate in clinical studies or surveys directly through the platform. By engaging in these research activities, you can contribute to cutting-edge studies that aim to advance eczema treatment and care.
- Contributing to Global Research Initiatives
The data collected through the Eczemaless App can be shared with global research initiatives focused on eczema. This collaborative effort enhances the scope and impact of eczema research, leading to a better understanding of the condition on a worldwide scale.
Conclusion
The Eczemaless App is a comprehensive tool designed to enhance your eczema care journey. With personalized management plans, comprehensive symptom tracking, access to expert advice, real-time progress monitoring, and a supportive community, the app offers everything you need to effectively manage your eczema. Don’t let eczema control your life—take charge of your care with the Eczemaless App today and experience the difference it can make in your skin health and overall well-being.
Track and Manage your Eczema treatment using a comprehensive Eczema App
Download Eczemaless now