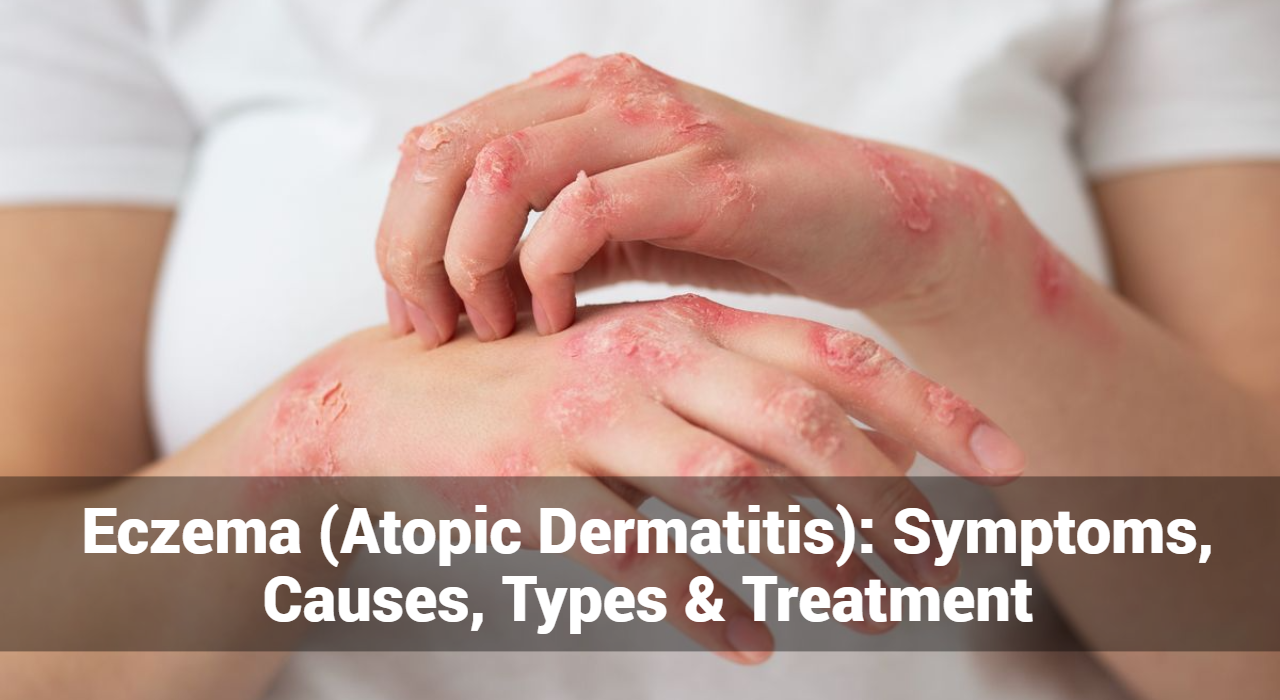
Eczema (Atopic Dermatitis): Symptoms, Causes, Types & Treatment
Eczema, also known as atopic dermatitis, is a common skin condition characterized by inflammation, itching, and irritation of the skin. It can affect people of all ages but is more prevalent in children. Eczema is not contagious, but it can be uncomfortable and cause distress. Here’s an overview of what eczema is, its symptoms, causes, types, and treatment options:
What Is Eczema (atopic dermatitis)?
Eczema is a chronic skin condition that causes inflammation and irritation of the skin. It is characterized by red, itchy, and inflamed patches of skin that may appear dry, scaly, or cracked. Eczema can occur anywhere on the body but is commonly found on the face, hands, feet, and behind the knees.
What are the Symptoms of Eczema?
Eczema, also known as atopic dermatitis, can manifest through various symptoms that affect the skin. Here are some common symptoms associated with eczema:
- Itching (Pruritus): One of the hallmark symptoms of eczema is intense itching, which can be relentless and may worsen at night. Scratching the affected areas can lead to further irritation and inflammation.
- Redness (Erythema): Eczema often causes patches of red, inflamed skin. These areas may appear darker or lighter than the surrounding skin and may be accompanied by warmth.
- Dryness: Eczema-prone skin tends to be dry and may feel rough or scaly to the touch. This dryness can contribute to itchiness and discomfort.
- Rashes: Eczema can cause various types of rashes, including:
- Eczematous (eczema) rash: Characterized by red or pink patches of skin that may be raised, bumpy, or scaly.
- Vesicular rash: Small, fluid-filled blisters that may ooze or crust over when scratched.
- Excoriated rash: Areas of broken skin resulting from scratching, which may be raw, weepy, or crusted.
- Thickened Skin (Lichenification): Chronic scratching or rubbing of the skin can lead to thickened, leathery patches known as lichenification. This often occurs in areas that are frequently scratched, such as the elbows, knees, and neck.
- Cracking and Flaking: In severe cases of eczema, the skin may crack or fissure, leading to pain, bleeding, and susceptibility to infections.
- Swelling (Edema): Eczema can cause swelling of the affected skin, which may be accompanied by a sensation of tightness or discomfort.
- Secondary Infections: Constant scratching can break the skin’s barrier, making it more susceptible to bacterial, viral, or fungal infections. Signs of infection include pus, increased pain, warmth, and redness.
- Discoloration: Prolonged eczema flare-ups may result in changes in skin color, such as hyperpigmentation (darkening) or hypopigmentation (lightening) of the affected areas.
It’s essential to note that eczema symptoms can vary in severity and may fluctuate over time. Additionally, individuals with eczema may experience symptoms differently, and some may have specific triggers that worsen their condition. If you or someone you know is experiencing symptoms of eczema, it’s crucial to consult a healthcare professional for an accurate diagnosis and appropriate management plan.
What causes eczema?
Eczema, also known as atopic dermatitis, is a complex condition with various contributing factors. While the exact cause of eczema is not fully understood, it is believed to result from a combination of genetic, environmental, and immune system factors. Here are some common factors that may contribute to the development of eczema:
- Genetics: Eczema tends to run in families, suggesting a genetic predisposition to the condition. Individuals with a family history of eczema, asthma, or hay fever are at a higher risk of developing eczema themselves.
- Abnormal Immune Response: Eczema is associated with an overactive immune response in the body, leading to inflammation and skin irritation. This immune dysregulation can result in the skin’s barrier function being compromised, making it more susceptible to irritants, allergens, and pathogens.
- Skin Barrier Dysfunction: People with eczema often have a compromised skin barrier, which allows irritants, allergens, and bacteria to penetrate the skin more easily. Factors such as dry skin, harsh soaps, hot water, and frequent bathing can further disrupt the skin barrier, exacerbating eczema symptoms.
- Environmental Triggers: Certain environmental factors can trigger or exacerbate eczema flare-ups. These triggers may include:
- Allergens: Common allergens such as dust mites, pet dander, pollen, and mold can trigger allergic reactions in susceptible individuals, leading to eczema flare-ups.
- Irritants: Harsh chemicals found in soaps, detergents, shampoos, and skincare products can irritate the skin and worsen eczema symptoms.
- Weather: Dry, cold weather can lead to dry skin, while hot, humid weather can cause sweating and irritation, both of which can trigger eczema flare-ups.
- Stress: Emotional stress and anxiety can exacerbate eczema symptoms in some individuals, although the exact mechanism is not fully understood.
- Microbial Factors: Bacterial, viral, and fungal infections can exacerbate eczema symptoms, especially in cases of severe eczema or when the skin barrier is compromised. Common infections associated with eczema include Staphylococcus aureus (staph) and herpes simplex virus (HSV).
It’s important to note that eczema triggers and causes can vary from person to person, and identifying individual triggers is essential for effective management. Additionally, managing eczema often involves a combination of lifestyle modifications, skincare practices, and medical treatments tailored to each individual’s needs. If you suspect you have eczema or are experiencing persistent skin issues, it’s important to consult a healthcare professional for an accurate diagnosis and personalized treatment plan.
GET IN CONTROL OF YOUR ECZEMA
Use our AI tool to check the severity of Eczema and keep track of your Eczema progress.
What are the types of eczema (atopic dermatitis)?
Eczema, also known as atopic dermatitis, can manifest in several different types, each with its own distinct characteristics. Here are some of the common types of eczema:
- Atopic Dermatitis: This is the most common form of eczema and often begins in infancy or childhood. It is characterized by dry, itchy skin and can be triggered or exacerbated by various factors, including allergens, irritants, stress, and climate changes.
- Contact Dermatitis: This type of eczema occurs when the skin comes into contact with irritants or allergens, leading to redness, itching, and inflammation. There are two subtypes of contact dermatitis:
- Irritant Contact Dermatitis: Caused by exposure to irritating substances such as soaps, detergents, chemicals, or harsh skincare products.
- Allergic Contact Dermatitis: Triggered by an allergic reaction to specific allergens, such as certain metals, latex, cosmetics, or plant extracts like poison ivy or poison oak.
- Dyshidrotic Eczema: Also known as pompholyx eczema, this type of eczema primarily affects the hands and feet. It is characterized by small, fluid-filled blisters (vesicles) that may be intensely itchy and can cause pain and discomfort.
- Nummular Eczema: Also called discoid eczema, this type of eczema is characterized by round or oval-shaped patches of red, inflamed skin that may ooze or crust over. These patches typically appear on the arms, legs, back, or buttocks and can be very itchy.
- Seborrheic Dermatitis: Although not strictly considered a type of eczema, seborrheic dermatitis shares some similarities with eczema. It primarily affects areas of the body with high sebum production, such as the scalp, face (particularly around the eyebrows, nose, and ears), and upper chest. It is characterized by red, scaly patches and may be accompanied by itching and flaking.
- Stasis Dermatitis: Also known as gravitational eczema, this type of eczema typically occurs in individuals with poor circulation or venous insufficiency. It commonly affects the lower legs and is characterized by redness, swelling, and skin discoloration, often accompanied by itching and pain.
- Neurodermatitis: Also called lichen simplex chronicus, this type of eczema is characterized by thickened, scaly patches of skin that result from repeated scratching or rubbing. It often develops in response to chronic itching and may occur anywhere on the body.
These are just a few examples of the types of eczema that individuals may experience. It’s essential to consult a healthcare professional for an accurate diagnosis and appropriate management plan if you suspect you have eczema or are experiencing eczema-like symptoms.
Eczema (atopic dermatitis) Treatment
Eczema treatment aims to manage symptoms, reduce inflammation, and prevent flare-ups. The specific approach to treatment may vary depending on the type and severity of eczema, as well as individual factors such as age and overall health. Here are some common treatments and strategies for managing eczema:
- Moisturizers: Regular and frequent application of moisturizers is crucial for managing eczema. Emollients help to hydrate the skin and restore the skin barrier function, reducing dryness and itchiness. Choose fragrance-free, hypoallergenic moisturizers and apply them liberally after bathing or whenever the skin feels dry.
- Topical Corticosteroids: These are anti-inflammatory medications available in various strengths and formulations, including creams, ointments, and lotions. Topical corticosteroids help reduce inflammation, itching, and redness associated with eczema flare-ups. They are usually applied to affected areas for a short period under the guidance of a healthcare professional.
- Topical Calcineurin Inhibitors: These medications, such as tacrolimus (Protopic) and pimecrolimus (Elidel), are non-steroidal anti-inflammatory creams or ointments. They are used for mild to moderate eczema and can be applied to sensitive areas like the face and neck to reduce inflammation and itching.
- Antihistamines: Oral antihistamines may be prescribed to help relieve itching and discomfort caused by eczema. They are particularly useful for managing nighttime itching, which can disrupt sleep.
- Wet Wrap Therapy: This involves applying a layer of moisturizer followed by a damp layer of clothing or bandages to the affected skin. Wet wrap therapy helps to lock in moisture and can be beneficial for severe eczema flare-ups, but it should be done under medical supervision.
- Phototherapy: Phototherapy, or light therapy, involves exposing the skin to controlled amounts of natural or artificial ultraviolet light. It can help reduce inflammation and itching in some cases of moderate to severe eczema.
- Systemic Medications: In cases of severe eczema that do not respond to other treatments, systemic medications such as oral corticosteroids, immunosuppressants, or biologic agents may be prescribed. These medications work by suppressing the immune system and reducing inflammation throughout the body.
- Identifying and Avoiding Triggers: It’s essential to identify and avoid triggers that can exacerbate eczema symptoms. Common triggers include certain foods, environmental allergens, harsh soaps or detergents, stress, and extremes of temperature or humidity.
- Skin Care Practices: Practice gentle skin care habits, such as using mild, fragrance-free cleansers, avoiding hot baths or showers, patting the skin dry instead of rubbing, and wearing soft, breathable fabrics.
- Stress Management: Stress can exacerbate eczema symptoms, so incorporating stress-reduction techniques such as mindfulness, relaxation exercises, or yoga into your daily routine may help manage eczema.
It’s essential to work closely with a healthcare professional, such as a dermatologist, to develop a personalized treatment plan that addresses your specific eczema symptoms and needs.
Track and Manage your Eczema treatment using a comprehensive Eczema App
Download Eczemaless now
Conclusion
Overall, eczema (atopic dermatitis) is a chronic condition that requires ongoing management, but with proper treatment and care, most people with eczema can lead healthy and comfortable lives. If you suspect you have eczema or have concerns about your skin health, it’s essential to consult with a dermatologist or healthcare professional for an accurate diagnosis and personalized treatment plan.



Use our AI tool to check the severity of Eczema and keep track of your Eczema progress
Recent Posts
- What Is Behcet’s Disease? – It’s Symptoms, Causes, & How to Treat
- Genital Psoriasis: Symptoms, Causes, and How to Treat It
- Nickel Allergy: Symptoms, Treatment & How to Protect Yourself
- Pregnancy Acne: Causes, Home Remedies, and How to Treat It
- 5 Reasons to Use the Eczemaless App for Your Eczema Care Today


