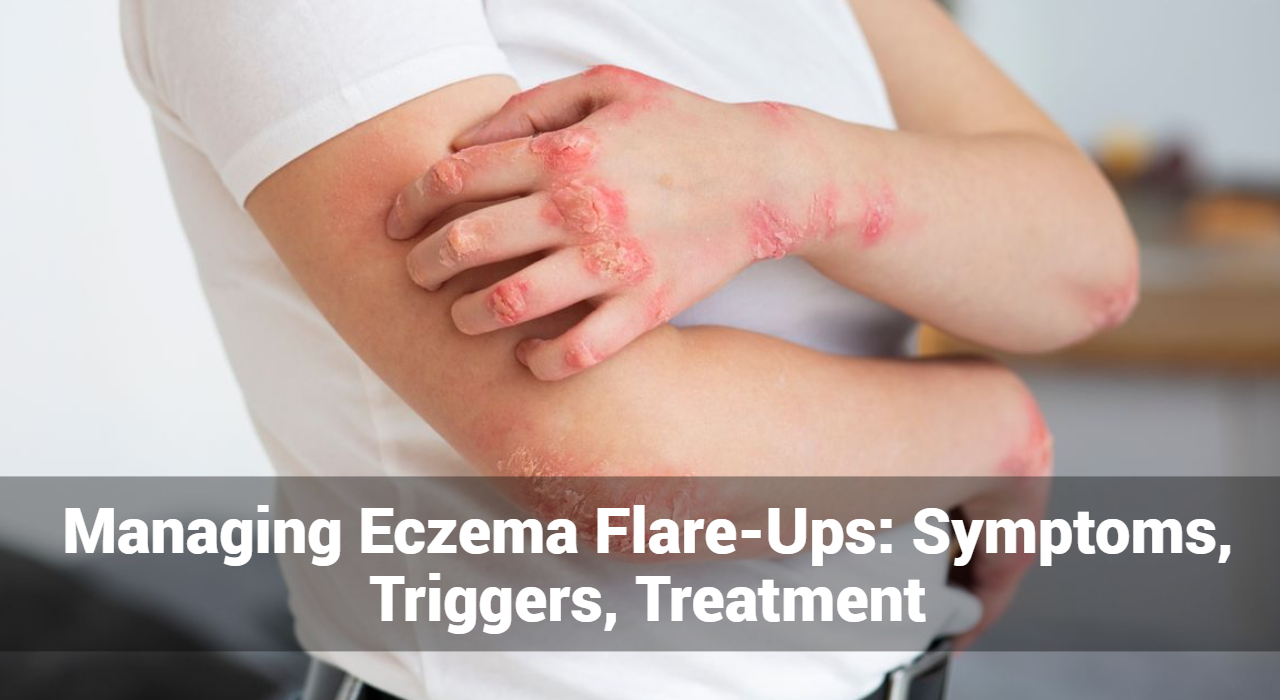
Eczema, also known as atopic dermatitis, is a chronic skin condition characterized by red, inflamed, and itchy patches of skin. Understanding the symptoms, triggers, and treatment options for eczema flare-ups is essential for effective management and relief.
What Is an Eczema Flare-Up?
An eczema flare-up refers to a sudden worsening of eczema symptoms, characterized by increased redness, inflammation, itching, and discomfort in the affected areas of the skin. During a flare-up, the skin becomes more irritated, dry, and prone to cracking or oozing. Eczema flare-ups can vary in severity and duration, ranging from mild to severe and lasting for several days or weeks. Triggers such as allergens, irritants, stress, weather changes, or hormonal fluctuations can provoke flare-ups in individuals with eczema. Managing eczema flare-ups involves identifying and avoiding triggers, maintaining proper skincare routines, using prescribed medications or treatments, and seeking medical advice when necessary to alleviate symptoms and prevent further exacerbation of the condition.
What Triggers Eczema Flare-Ups?
Eczema flare-ups can be triggered by various factors, and identifying these triggers is crucial for managing the condition effectively. Some common triggers of eczema flare-ups include:
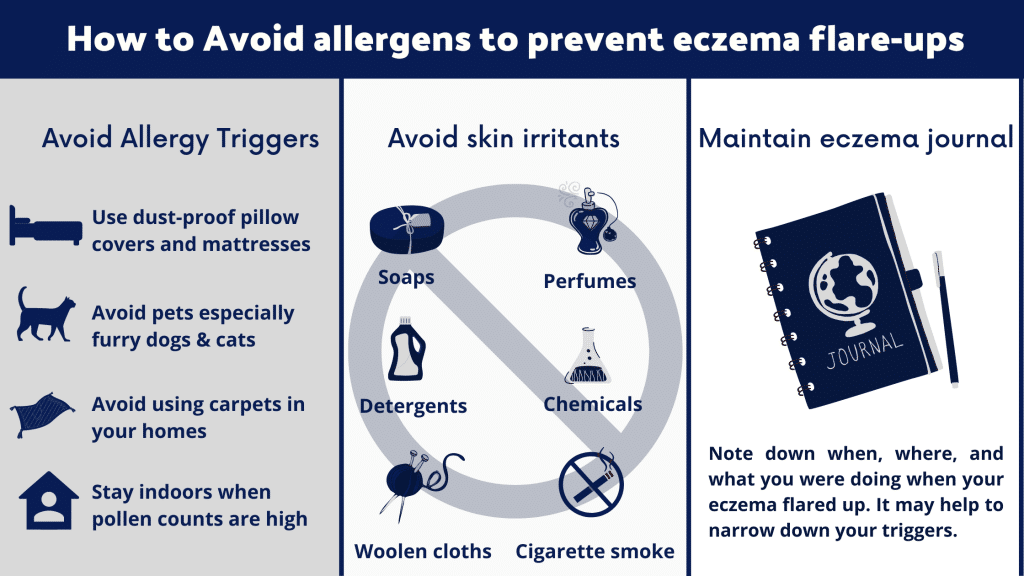
- Allergens: Exposure to allergens such as pollen, pet dander, dust mites, mold, or certain foods can trigger allergic reactions in individuals with eczema, leading to flare-ups.
- Irritants: Contact with irritants like harsh soaps, detergents, shampoos, perfumes, or chemicals can irritate the skin and trigger eczema flare-ups.
- Weather Changes: Extremes in temperature, humidity, or dryness can exacerbate eczema symptoms. Cold weather, low humidity levels, or excessive heat can all trigger flare-ups.
- Stress: Emotional stress, anxiety, or tension can weaken the immune system and increase inflammation in the body, leading to eczema flare-ups.
- Hormonal Changes: Hormonal fluctuations, such as those occurring during puberty, pregnancy, menstruation, or menopause, can trigger eczema flare-ups in some individuals.
- Skin Irritation: Friction from tight clothing, scratching, rubbing, or excessive bathing can irritate the skin and worsen eczema symptoms.
- Microbial Infections: Bacterial, viral, or fungal infections can cause inflammation and aggravate eczema symptoms, leading to flare-ups.
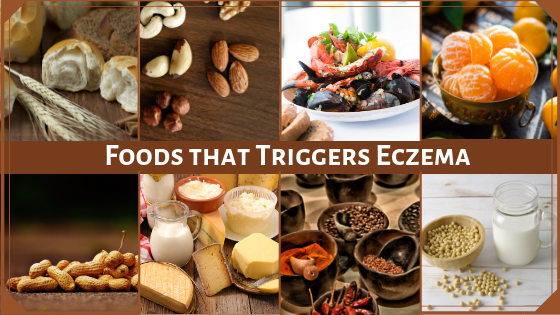
- Diet: Certain foods and food allergies can trigger eczema flare-ups in some individuals. Common triggers include dairy products, eggs, nuts, soy, wheat, and seafood.
- Environmental Factors: Indoor or outdoor pollutants, smoke, air pollution, or exposure to chemicals can irritate the skin and trigger eczema flare-ups.
- Medications: Some medications, such as antibiotics, antihistamines, or painkillers, may exacerbate eczema symptoms as a side effect in some individuals.
Identifying and avoiding these triggers, practicing good skincare habits, moisturizing regularly, and using prescribed medications or treatments can help manage eczema flare-ups effectively. Additionally, consulting with a healthcare professional or dermatologist for personalized advice and treatment recommendations is essential for individuals with eczema.
Track and Manage your Eczema treatment using a comprehensive Eczema App
Download Eczemaless now
How to Treat Eczema Flares?
Treating eczema flares involves a combination of preventive measures, skincare practices, and medical treatments to manage symptoms effectively. Here are some strategies for treating eczema flares:
- Moisturize Regularly: Keep the skin well-hydrated by applying moisturizers frequently, especially after bathing or showering. Use fragrance-free and hypoallergenic moisturizers to avoid irritation.
- Avoid Triggers: Identify and avoid triggers that can exacerbate eczema symptoms, such as allergens, irritants, stress, weather changes, and certain foods.
- Gentle Skincare: Use mild, fragrance-free cleansers and skincare products that are specifically formulated for sensitive skin. Avoid harsh soaps, detergents, and skincare products that contain alcohol or fragrances.
- Bathe Wisely: Take short, lukewarm baths or showers using gentle, non-soap cleansers. Pat the skin dry with a soft towel and avoid rubbing, which can irritate the skin.
- Topical Treatments: Apply over-the-counter or prescription topical corticosteroids to reduce inflammation and itching during eczema flares. Nonsteroidal options like calcineurin inhibitors may also be prescribed.
- Anti-Itch Medications: Over-the-counter antihistamines can help alleviate itching associated with eczema flares. Consult a healthcare professional before using any medication, especially for children.
- Wet Wrap Therapy: Wet wrap therapy involves applying a moisturizer or topical medication to the skin, followed by wrapping the affected area with dampened bandages or clothing. This can help soothe the skin and enhance the absorption of topical treatments.
- Avoid Scratching: Encourage gentle scratching or patting instead of vigorous rubbing or scratching, which can further irritate the skin and lead to infection.
- Cool Compresses: Apply cool, damp compresses or ice packs to the affected areas to help relieve itching and reduce inflammation during eczema flares.
- Prescription Medications: In severe cases of eczema, oral medications such as oral corticosteroids, immunosuppressants, or biologics may be prescribed by a healthcare professional to manage symptoms and prevent flares.
- Phototherapy: Phototherapy or light therapy involves exposing the skin to ultraviolet (UV) light under medical supervision to reduce inflammation and itching associated with eczema flares.
It’s essential to work closely with a dermatologist or healthcare professional to develop a personalized treatment plan for managing eczema flares effectively. They can provide guidance on the most appropriate treatments based on the severity of symptoms and individual needs.
Common symptoms of eczema flare-ups include:
- Intense Itching: Itching is often the most prominent symptom of eczema flare-ups and can be relentless, leading to scratching and further irritation of the skin.
- Redness and Inflammation: The affected skin may appear red, inflamed, and swollen during flare-ups, indicating increased inflammation in the affected area.
- Dryness and Scaling: Eczema flare-ups are often accompanied by dry, scaly patches of skin, which can become rough, cracked, and painful.
- Rash and Blisters: Rash-like patches may develop on the skin during flare-ups, accompanied by small fluid-filled blisters that can rupture and weep.
- Skin Thickening: Prolonged or repeated scratching of the skin during flare-ups can lead to thickening and hardening of the skin, known as lichenification.
Treatment Options for Eczema Flare-Ups:
Managing eczema flare-ups requires a multifaceted approach that addresses both the underlying causes of the condition and the immediate symptoms. Here are some treatment options for eczema flare-ups:
- Moisturizers: Regularly moisturizing the skin is essential for managing eczema flare-ups. Use emollients or moisturizers that are fragrance-free, hypoallergenic, and suitable for sensitive skin.
- Topical Corticosteroids: Topical corticosteroids are commonly prescribed to reduce inflammation and itching during eczema flare-ups. They help to alleviate symptoms and promote healing of the skin.
- Topical Calcineurin Inhibitors: Calcineurin inhibitors are non-steroidal medications that help to reduce inflammation and itching associated with eczema flare-ups. They are often used as an alternative to corticosteroids, especially on sensitive areas of the skin.
- Antihistamines: Oral antihistamines may be recommended to relieve itching and discomfort during eczema flare-ups. They help to block the action of histamine, a chemical involved in the inflammatory response.
- Wet Wrap Therapy: Wet wrap therapy involves applying moisturizer or medication to the skin, followed by wrapping the affected area with damp bandages or clothing. This helps to hydrate the skin and enhance the absorption of topical treatments.
- Avoiding Triggers: Identify and avoid triggers that can exacerbate eczema flare-ups, such as certain fabrics, harsh soaps, and environmental allergens.
- Prescription Medications: In severe cases of eczema flare-ups, prescription medications such as oral corticosteroids or immunosuppressants may be prescribed by a dermatologist to help control symptoms.
Conclusion:
Eczema flare-ups can be challenging to manage, but with the right approach, symptoms can be alleviated effectively. By understanding the symptoms of eczema flare-ups and exploring various treatment options, individuals can find relief and improve their quality of life. If you or a loved one is experiencing eczema flare-ups, consult a dermatologist for personalized treatment recommendations.
GET IN CONTROL OF YOUR ECZEMA
Use our AI tool to check the severity of Eczema and keep track of your Eczema progress.