Index
Environment and Eczema
Though the exact causes of Eczema (Atopic Dermatitis) are unclear it is widely accepted that Eczema is aggravated by a combination of genetic and environmental factors. Eczema flareups are due to defensive actions of the immune response cells of the body reacting to foreign factors. These foreign factors are called triggers. These triggers can be apparently harmless aspects of your daily life. Some of these triggers can be controlled by patients but many of them are beyond their easy control. Triggers such as specific food ingredients, clothes, perfumes, etc can be controlled or avoided easily. However, some triggers such as pollen count, humidity, temperature, etc. are beyond a patient’s control or cannot be avoided easily. Some of the weather and other environmental triggers have a dramatic impact on the severity of an eczema flare-up.
Our skin is the outermost organ of our body which senses conditions and adapts accordingly for e.g. if the climate is hot it perspires to make it cool and has a layer of fat under it to keep the body warm in cold weather. But these adaptation functions of the skin despair to an extent in people with Atopic Dermatitis The skin affected with eczema loses more water than it should and gives an open ground for microbes, allergens, and other irritants. Climate or weather affects each person differently even if two individuals are suffering from Atopic Dermatitis both of them will react differently to different triggers. The exact relationship between weather and Eczema has not been defined, but experts consider that the damage to the skin’s barrier may hamper the ability to adapt to the changing weather. Let’s check out some important environmental factors and how do they affect eczema.
Try Eczemaless an AI app to keep a check on the most common weather triggers such as temperature, pollen, humidity, etc that cause eczema flares.
Get your Eczema severity score and keep track of your Eczema progress.
– Humidity
Humidity is one of the vital factors in the environment, to which skin reacts almost immediately and it plays a major role in how your body handles eczema.
Dry and Low humidity: The dry air pulls moisture from the skin making it dry worsening the eczema plaques further.
Hot and High humidity: The hot and sticky climate makes your skin sweat a lot making eczema-prone skin itchier and more irritated resulting in a flare-up
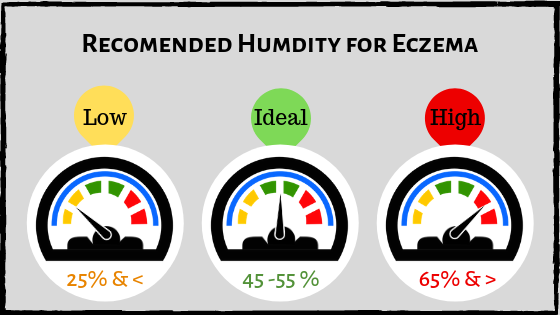
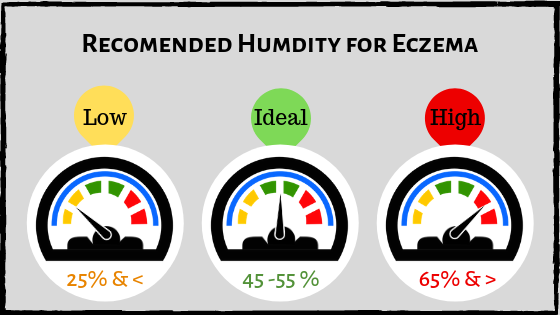
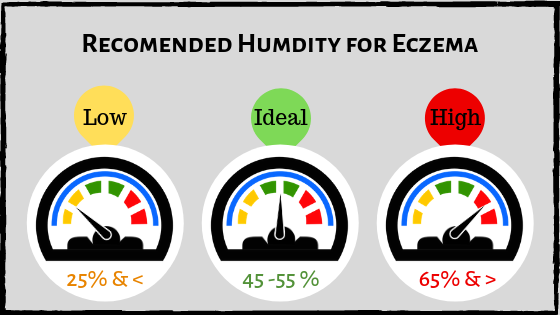
A perfect level of humidity can be different for each person but climate with 50% humidity in the air is ideal. Both Low and High humidity is bad for eczema wherein Low humidity triggers your eczema or intensifies a flare-up, whereas hot weather worsens an existing outbreak intensifying the itch.
Tips
- If possible and feasible with your work-life balance, move to a place better suited for your eczema
- Take necessary precaution while moving out of home and try avoiding a condition in which you will sweat more such as congested rooms or trains.
- use humidifiers/dehumidifiers and indoor AC/heating, to control the climate at least inside homes and set it at an ideal condition for eczema
– Winter
Experts found that people with Eczema experience greater itchiness in cold weather than summer season and that maybe the reason your flare-ups occur predominantly in winter. Changes between cold and hot environments also worsen Eczema.
The combined effect of low temperatures, less humidity and dry air with a reduced or negligible amount of sunshine in winter aggravates eczema flare. The dry air drains and evaporates moisture from the skin making it dry and triggering a flare. Low temperatures demand insulation which comes in the form of increased clothing. Some of the warm clothing is made from wool and other fibers which reduce ventilation of skin and also cause irritation increasing the itch and need for scratching worsening eczema.
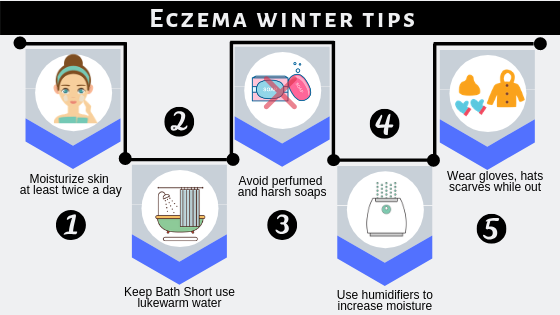
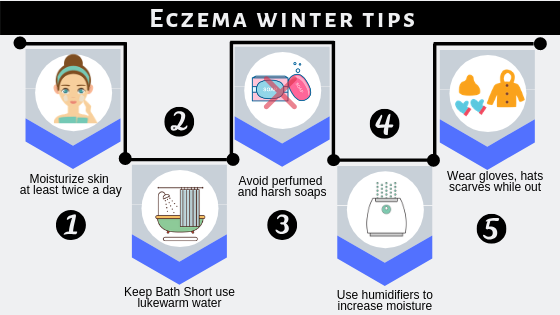
Tips
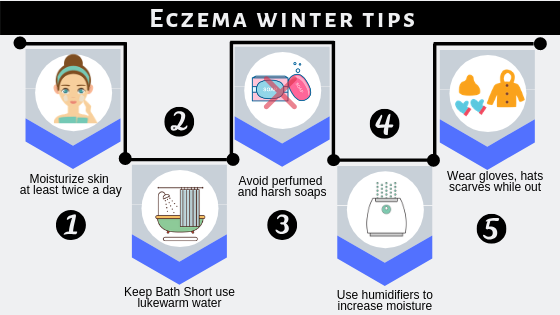
- Moisturize skin at least twice a day. Lock the moisture in the skin to help hydration and repair the skin barrier
- Use lukewarm water for bathing and keep baths short.
- Avoid harsh soaps, which can further dry and irritate the skin
- Use humidifiers to increase the amount of moisture in the room.
- Wear suitable clothes while going outside. Hats, scarves, and gloves may be required but avoid those made from wool, which can increase itching and scratching.
– Heat
When an eczema patient is exposed to heat, and the temperature reaches a certain level, it gives an itching sensation exacerbating eczema. The normal mechanism of the body’s sweating in hot condition to cool down actually worsens the condition in eczema. Moreover, when the sweat evaporates leaves the sodium in the skin making it drier and itchier.
Apart from hot weather conditions other causes that overheat the body include exercising, wearing non-breathable fabrics and overdressing
Tips
- Avoid Overheating
- Avoid overdressing, wear breathing fabric such as cotton.
- put on moisturizers and sunblock when outside, and try not to get into situations where you sweat
Take a shower after exercise or whenever you sweat a lot due to traveling, playing, etc.
– Sunlight
Sun acts as both the healer and as a culprit for Eczema flares.
Sunlight can act as a treatment for eczema. People with severe cases can benefit from ultraviolet ray treatments. Sun exposure leads to increased vitamin D production, which can be great for the health of the skin.
For Many people Sun can be an irritant and may cause you sunburn and be a reason for increasing your itch, raising your body temperature, causing you sweat ultimately causing your eczema flare.
Tips
- use an eczema-safe sunscreen when in sun for extended periods.
- shield yourself with breathable clothes and a hat.
– Pollutants
Pollution or pollutants don’t directly cause Eczema but definitely can be a trigger that may cause an eczema flare worsening the condition. The correlation between air pollution and the prevalence and severity of atopic dermatitis is well known. The mechanism behind this is, itch causes scratching, disrupting the skin barrier function, and opening the entry for antigens (pollutants) to penetrate. This results in the patients being sensitized to antigens and subject to allergic diseases, in this case, Atopic Dermatitis.
This apart you may also be subjected to indoor allergens such as dust mites, pet dander, Pollen, mold, etc.
If allergies are a trigger for your eczema, take steps to control them.
Tips
- Keep your home clean. Dust often and be sure to vacuum carpets frequently.
- Get rid of dust mites by washing bedding, curtains, blankets, etc. at least fortnightly with very hot water.
- Keep pets out of your bedroom
- Close your windows during peak allergy season to avoid exposure to mold and pollen
To live a healthy life with eczema it is important to keep your symptoms and triggers under check. While tracking Eczema triggers keep in mind that eczema flare can appear even after some time to exposure, the lag time appears as a challenge to narrow down the trigger.
Approach a Physician
In case your eczema suddenly gets out of control it could be possible that you have developed an allergy or an Infection. In such case better to approach for medical health.
It is also advisable to approach a dermatologist if your symptoms are proving very hard to manage on your own.
Take away
As already mentioned, under tips section of each category of environmental factors, the best way to deal with your local weather is to move to a weather location less averse to Eczema and wear appropriate clothes, put on moisturizers and sunblock when leaving the house, and avoid situations which will make you sweat. Make sure that your bedroom is at the perfect level of humidity and heat using humidifier/dehumidifier, AC / heater, etc. This ensures that you will be more comfortable at least when you sleep and help keep eczema flare-ups calm through the night.
Try out EczemaLess App to keep a track of Environmental Triggers as the app automatically records the most common weather triggers such as pollen, humidity, etc. Users can log suspected triggers through the intuitive user interface. The app comes pre-populated with the most common triggers, users can add custom triggers.