Hand eczema, a common dermatological condition, manifests in various forms, each requiring tailored treatment approaches for effective management. This concise guide aims to shed light on seven distinct types of hand eczema and provide insights into treating each one effectively.
What is Hand Eczema?
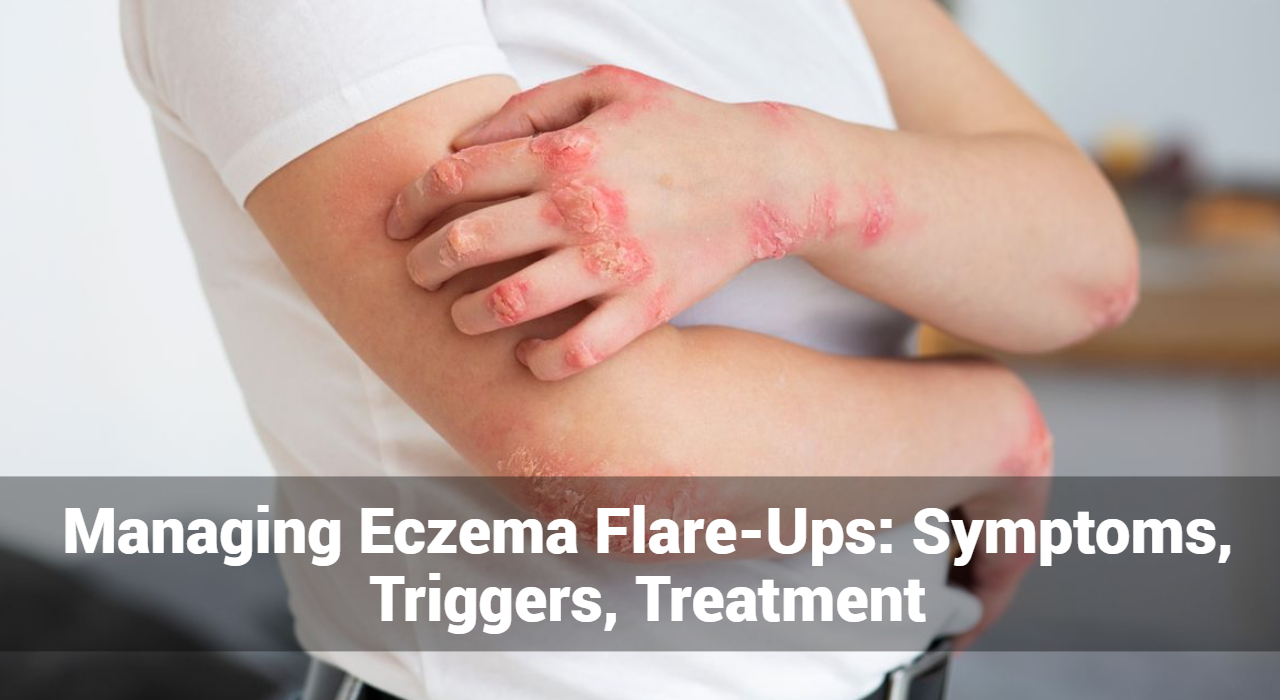
Hand eczema, also known as hand dermatitis, refers to a skin condition characterized by inflammation, dryness, redness, itching, and sometimes blistering on the hands. It can vary in severity from mild irritation to debilitating discomfort. Hand eczema can be caused by a combination of genetic, environmental, and lifestyle factors.
There are several types of hand eczema, including atopic dermatitis (AD), contact dermatitis, dyshidrotic eczema, nummular eczema, seborrheic dermatitis, stasis dermatitis, and occupational eczema. Each type has its own specific triggers and symptoms, but they generally involve some degree of inflammation and irritation of the skin on the hands.
Common triggers for hand eczema include exposure to irritants such as soaps, detergents, chemicals, and allergens like metals, latex, or certain plants. Other factors such as stress, dry weather, frequent hand washing, and genetic predisposition can also contribute to the development or exacerbation of hand eczema.
Common 7 Types of Hand Eczema
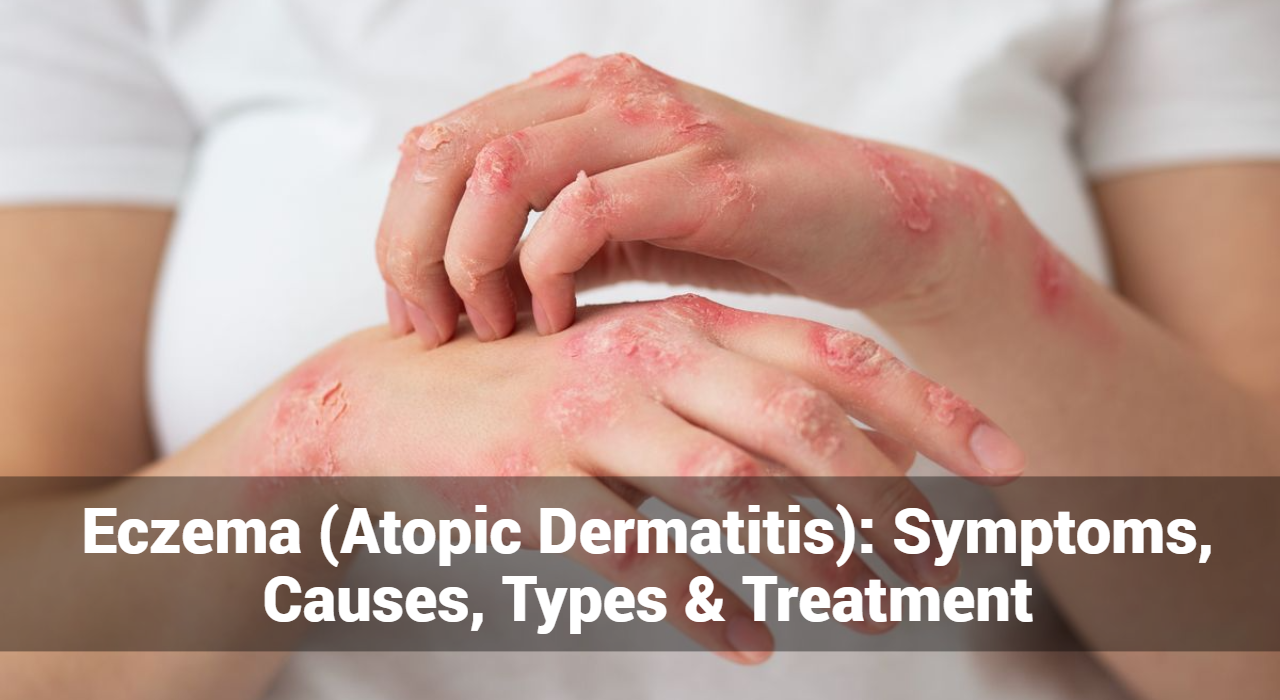
#01. Atopic Dermatitis (AD):
-
- A chronic inflammatory skin condition characterized by dry, itchy, and inflamed skin. It often appears in childhood and may persist into adulthood, with flare-ups triggered by allergens, stress, or environmental factors.
How To Treatment of Atopic Dermatitis (AD):
-
-
- Use gentle, fragrance-free cleansers and moisturizers to hydrate the skin.
- Apply topical corticosteroids or immunomodulators to reduce inflammation during flare-ups.
- Identify and avoid triggers such as harsh soaps, detergents, and allergens.
- Practice stress management techniques as stress can exacerbate symptoms.
-
#02. Contact Dermatitis:
-
- Contact dermatitis occurs when the skin comes into contact with irritants or allergens, leading to redness, itching, and sometimes blistering. Common triggers include chemicals, soaps, metals, and certain plants.
How To Treatment of Contact Dermatitis:
-
-
- Identify and avoid contact with irritants or allergens.
- Use protective gloves when handling chemicals or working with materials known to trigger a reaction.
- Apply topical corticosteroids or barrier creams to soothe and protect the skin.
- Practice proper hand hygiene to prevent further irritation.
-
Track and Manage your Eczema treatment using a comprehensive Eczema App
Download Eczemaless now
#03. Dyshidrotic Eczema:
-
- Dyshidrotic eczema primarily affects the palms, fingers, and soles of the feet. It causes small, itchy blisters and can be triggered by stress, sweating, or exposure to allergens like metals or certain foods.
How To Treatment of Dyshidrotic Eczema:
-
- Keep the hands clean and dry to prevent moisture buildup.
- Apply cool compresses to reduce itching and inflammation.
- Use topical corticosteroids or immunomodulators to reduce blistering and inflammation.
- Avoid potential triggers such as stress, sweating, and exposure to allergens.
#04. Nummular Eczema:
-
- Nummular eczema presents as coin-shaped patches of irritated, inflamed skin. These patches may be itchy, scaly, and can ooze fluid. They often occur after skin injuries or in individuals with dry skin.
How To Treatment of Nummular Eczema:
-
- Moisturize regularly to hydrate the skin and prevent dryness.
- Apply topical corticosteroids or calcineurin inhibitors to reduce inflammation.
- Avoid scratching to prevent further irritation and potential infection.
- Identify and avoid triggers such as dry weather, harsh soaps, and allergens.
#05. Seborrheic Dermatitis:
-
- Seborrheic dermatitis affects oily areas of the skin, including the scalp, face, and hands. It causes redness, scaling, and itching, and is often associated with dandruff and fungal infections.
How To Treatment of Seborrheic Dermatitis:
-
- Use medicated shampoos containing ingredients like ketoconazole or selenium sulfide to control scalp symptoms.
- Apply topical antifungal creams or corticosteroids to affected areas on the hands.
- Avoid triggers such as stress, cold weather, and certain foods that may exacerbate symptoms.
#06. Stasis Dermatitis:
-
- Stasis dermatitis develops due to poor circulation, typically in the lower legs and hands. It causes swollen, itchy, and discolored skin, often accompanied by pain and ulceration, and is common in individuals with venous insufficiency.
How To Treatment of Stasis Dermatitis:
-
- Elevate the affected hand(s) to improve circulation and reduce swelling.
- Wear compression garments to improve venous return and reduce fluid buildup.
- Apply moisturizers to hydrate the skin and prevent dryness and cracking.
- Treat underlying venous insufficiency with medications or procedures as recommended by a healthcare professional.
#07. Occupational Eczema:
-
- Occupational eczema is caused by exposure to irritants or allergens in the workplace. It can affect various industries, including healthcare, food handling, and cleaning. Symptoms resemble those of contact dermatitis and may require changes in work practices or protective measures.
How To Treatment of Occupational Eczema:
-
- Identify and eliminate or minimize exposure to workplace irritants or allergens.
- Use protective equipment such as gloves, barrier creams, or moisturizing lotions to prevent contact with irritants.
- Practice good hand hygiene and moisturize regularly to maintain skin barrier function.
- Consider occupational health assessments and adjustments to minimize exposure risks.
Identifying the specific type of hand eczema is essential for developing an effective treatment plan. Consulting a dermatologist can help in proper diagnosis and management strategies tailored to individual needs.
GET IN CONTROL OF YOUR ECZEMA
Use our AI tool to check the severity of Eczema and keep track of your Eczema progress.
Home Remedies for Hand Eczema
Home remedies can be helpful in managing mild cases of hand eczema or complementing medical treatments. Here are some home remedies to try:
- Oatmeal Baths:
- Add colloidal oatmeal to lukewarm bathwater and soak your hands for 15-20 minutes. Oatmeal has anti-inflammatory properties that can soothe irritated skin.
- Coconut Oil:
- Apply virgin coconut oil to your hands as a natural moisturizer. Coconut oil contains fatty acids that help hydrate and protect the skin barrier.
- Aloe Vera Gel:
- Apply pure aloe vera gel to the affected areas to reduce inflammation and soothe itching. Aloe vera has cooling and moisturizing properties.
- Apple Cider Vinegar:
- Dilute apple cider vinegar with water and apply it to your hands using a cotton ball. Apple cider vinegar has antimicrobial properties and may help reduce itching and inflammation.
- Cold Compresses:
- Apply a cold compress or ice pack wrapped in a towel to the affected areas to reduce itching and inflammation. Cold temperatures can numb the skin and provide temporary relief.
- Proper Hand Hygiene:
- Use mild, fragrance-free soap and lukewarm water to wash your hands, and pat them dry gently with a soft towel. Avoid hot water and harsh soaps, which can further dry out the skin.
- Moisturize Regularly:
- Apply a thick, fragrance-free moisturizer to your hands several times a day, especially after washing or bathing. Look for products containing ingredients like ceramides, glycerin, or petrolatum to lock in moisture.
- Wear Gloves:
- Protect your hands from harsh chemicals, detergents, and other irritants by wearing cotton gloves underneath rubber or vinyl gloves when doing household chores or working with potentially irritating substances.
- Avoid Triggers:
- Identify and avoid triggers that worsen your hand eczema, such as certain foods, allergens, or environmental factors like cold weather or dry air.
- Stress Management:
- Practice relaxation techniques such as deep breathing, meditation, or yoga to reduce stress levels, as stress can exacerbate eczema symptoms.
It’s important to note that while home remedies can provide relief for mild symptoms, they may not be sufficient for severe or persistent cases of hand eczema. If your symptoms worsen or do not improve with home care, consult a dermatologist or healthcare professional for proper diagnosis and treatment. They can recommend medical interventions such as topical medications, oral medications, or phototherapy as needed.
Conclusion
Understanding the diverse manifestations of hand eczema is crucial for targeted treatment and symptom management. By identifying the specific type of eczema and implementing appropriate interventions, individuals can alleviate discomfort and enhance the health of their skin. Remember, consulting a dermatologist for personalized guidance is always advisable for effective management of hand eczema.
Track and Manage your Eczema treatment using a comprehensive Eczema App
Download Eczemaless now