Cherry angiomas, also known as senile angiomas or Campbell de Morgan spots, are benign skin growths that can appear as small, red or purple spots on the skin. Although they are harmless, their appearance can be concerning to many individuals. In this article, we will explore the causes, symptoms, treatment options, and removal methods associated with cherry angiomas to provide a comprehensive understanding of this common skin condition.
What is a Cherry Angioma?
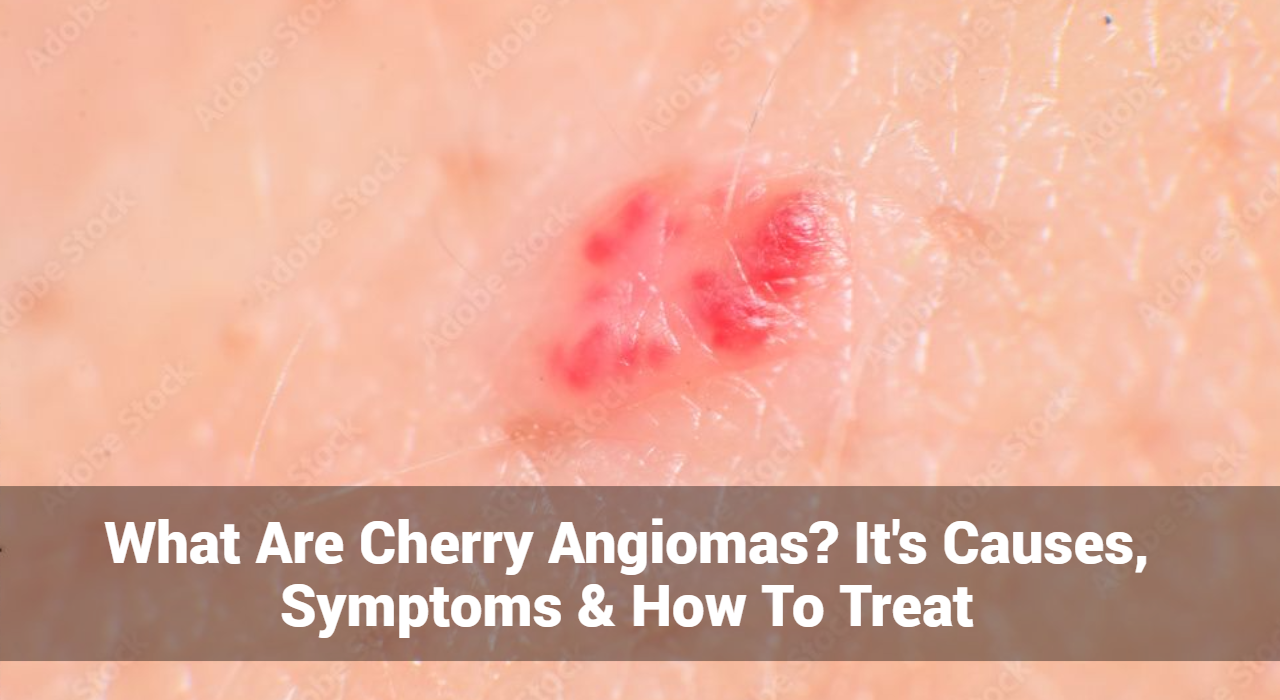
A cherry angioma is a type of vascular lesion that results from the proliferation of small blood vessels (capillaries) in the skin. These growths are usually bright red, but they can also appear blue or purple. They are most commonly found on the trunk, arms, and shoulders, but they can develop anywhere on the body.
Characteristics of Cherry Angiomas
- Color: Typically bright red but may appear purple or blue.
- Size: Usually small, ranging from a pinpoint to about a quarter of an inch in diameter.
- Texture: Smooth and dome-shaped, but they can also be flat.
- Location: Commonly found on the torso, arms, and neck, but they can occur anywhere on the body.
Track and Manage your Eczema treatment using a comprehensive Eczema App
Download Eczemaless now
What Causes of Cherry Angiomas?
Cherry angiomas are benign growths that typically appear as small, red, or purple spots on the skin. While the exact cause of cherry angiomas is not fully understood, several factors have been identified that may contribute to their development. Here’s a closer look at these potential causes:
- Family History: Cherry angiomas tend to run in families, suggesting a genetic predisposition. If your parents or siblings have cherry angiomas, you may be more likely to develop them as well.
- Incidence Increases with Age: The likelihood of developing cherry angiomas increases with age, particularly in individuals over 30. This age-related prevalence suggests that as the skin ages, its structure and blood vessels may become more susceptible to the formation of these growths.
- Pregnancy and Hormonal Fluctuations: Changes in hormone levels, such as during pregnancy, can trigger the development of cherry angiomas. Hormonal shifts may affect blood vessel growth and skin changes, leading to the appearance of these angiomas.
- Chemical Exposure: While specific environmental triggers have not been conclusively identified, some studies suggest that exposure to certain chemicals or irritants could contribute to the development of cherry angiomas. For instance, prolonged exposure to solvents or other chemical agents may play a role.
- Injury or Irritation: Some individuals report that cherry angiomas developed after skin trauma or irritation. While the connection isn’t definitively established, physical damage to the skin could potentially trigger the growth of these vascular lesions.
- Certain Health Conditions: In some cases, cherry angiomas may be associated with underlying medical conditions, such as hormonal disorders. However, this is less common, and the majority of cherry angiomas occur in otherwise healthy individuals.
GET IN CONTROL OF YOUR ECZEMA
Use our AI tool to check the severity of Eczema and keep track of your Eczema progress.
What Are The Symptoms of Cherry Angiomas?
While they typically do not cause significant symptoms, there are several characteristics and signs associated with cherry angiomas that individuals may observe. Here are the main symptoms:
1. Appearance
- Color: Cherry angiomas are usually bright red but can also appear purple or blue.
- Size: They typically range from a few millimeters to about a quarter of an inch in diameter.
- Shape: Most cherry angiomas have a smooth, dome-shaped surface, although some may be flat or slightly raised.
- Texture: The surface is usually smooth, but they can also be rough or scabby in some cases.
2. Location
- Common Areas: Cherry angiomas commonly appear on the trunk, arms, shoulders, and neck but can develop anywhere on the body, including the face and scalp.
3. Bleeding
- Injury: Cherry angiomas can bleed if they are accidentally scraped or cut. While they usually do not cause pain, bleeding can be a concern if the growth is injured.
- Spontaneous Bleeding: In rare cases, individuals may experience spontaneous bleeding from a cherry angioma, which may require medical attention.
4. Change in Size or Color
- Growth Over Time: Cherry angiomas may gradually increase in size or number over time. While this is common, any sudden changes in size, shape, or color should be evaluated by a healthcare professional.
- Color Changes: Some individuals may notice a darkening of the angioma over time.
5. Itching or Irritation (Rare)
- Mild Discomfort: Although cherry angiomas are typically painless, some individuals may experience mild itching or irritation, especially if the angioma is located in an area that experiences friction or irritation from clothing.
6. Psychological Impact
Cosmetic Concerns: The appearance of cherry angiomas can lead to self-consciousness or concerns about one’s appearance, especially if they are numerous or located on visible areas of the body.
Diagnosis of Cherry Angiomas
Diagnosing a cherry angioma typically involves a physical examination by a healthcare provider or consult a dermatologist. In most cases, no additional testing is necessary. However, if there is any doubt about the diagnosis, a biopsy may be performed to ensure that the growth is benign.
GET IN CONTROL OF YOUR ECZEMA
Use our AI tool to check the severity of Eczema and keep track of your Eczema progress.
What Are The Treatment Options for Cherry Angiomas?
While cherry angiomas are harmless and do not require treatment, some individuals choose to have them removed for cosmetic reasons. Several treatment options are available:
1. Laser Therapy: Laser therapy is a common method for removing cherry angiomas. A concentrated beam of light targets the blood vessels, causing them to collapse and fade. This treatment is quick and often requires little to no downtime.
2. Cryotherapy: Cryotherapy involves freezing the cherry angioma with liquid nitrogen. This process destroys the abnormal blood vessels, causing the growth to fall off after a few days.
3. Electrosurgery: In this method, a high-frequency electrical current is used to burn off the cherry angioma. This treatment can be effective for larger growths.
4. Surgical Excision: For larger or multiple cherry angiomas, surgical excision may be performed. This involves cutting out the growth with a scalpel, followed by suturing the skin. This method is often reserved for cases where other treatments are not suitable.
Home Remedies for Cherry Angiomas
While medical treatments are the most effective way to remove cherry angiomas, some home remedies may help improve their appearance or prevent new ones from forming:
- Apple Cider Vinegar: Applying apple cider vinegar to the angioma may help reduce its size over time.
- Tea Tree Oil: This essential oil is believed to have properties that may help reduce the appearance of cherry angiomas when applied topically.
- Healthy Lifestyle: Maintaining a balanced diet, staying hydrated, and protecting the skin from excessive sun exposure can promote overall skin health.
When to See a Doctor
While cherry angiomas are usually harmless, individuals should seek medical advice if they notice any of the following:
- Rapid Changes: Sudden changes in size, shape, or color of the angioma.
- Excessive Bleeding: Bleeding that does not stop or occurs frequently.
- New Growths: The development of new skin growths that differ in appearance from existing cherry angiomas.
- Associated Symptoms: Any discomfort, pain, or unusual symptoms associated with the angioma.
Prevention of Cherry Angiomas
Since the exact cause of cherry angiomas is not fully understood, there is no guaranteed way to prevent them. However, some general tips for maintaining healthy skin include:
- Sun Protection: Use sunscreen to protect your skin from harmful UV rays.
- Healthy Diet: A diet rich in fruits, vegetables, and antioxidants may contribute to skin health.
- Avoid Harsh Chemicals: Limit exposure to chemicals and irritants that may affect skin health.
Conclusion
Cherry angiomas are common, benign skin growths that can occur as people age. While they are generally harmless, many individuals seek treatment for cosmetic reasons. Understanding the causes, symptoms, and available treatment options can help individuals make informed decisions about their skin health. If you have concerns about cherry angiomas or any changes in your skin, it is always best to consult a healthcare professional for proper evaluation and advice.
By staying informed about cherry angiomas and maintaining good skin care practices, individuals can navigate this common skin condition with confidence.
Track and Manage your Eczema treatment using a comprehensive Eczema App
Download Eczemaless now