Table of Content
Introduction
Flare is a term commonly associated with Eczema. What is a Flare? A ‘flare’ or ‘flare-up’ is a term used in both medical and non-medical literature to refer to an exacerbation of a disease. Once someone has a flareup they start searching for a remedy to cure the flares. But perhaps it is more important to know what caused the flareup in the first place because as the adage goes “Prevention is better than cure.” Usually, Eczema flares are caused by some triggers. There is a list of commonly known triggers. Avoiding these common triggers can prevent a flare-up and the associated symptoms. Once you know what triggers flare your eczema, the best thing to do is to avoid those flares.
What Causes a Flare?
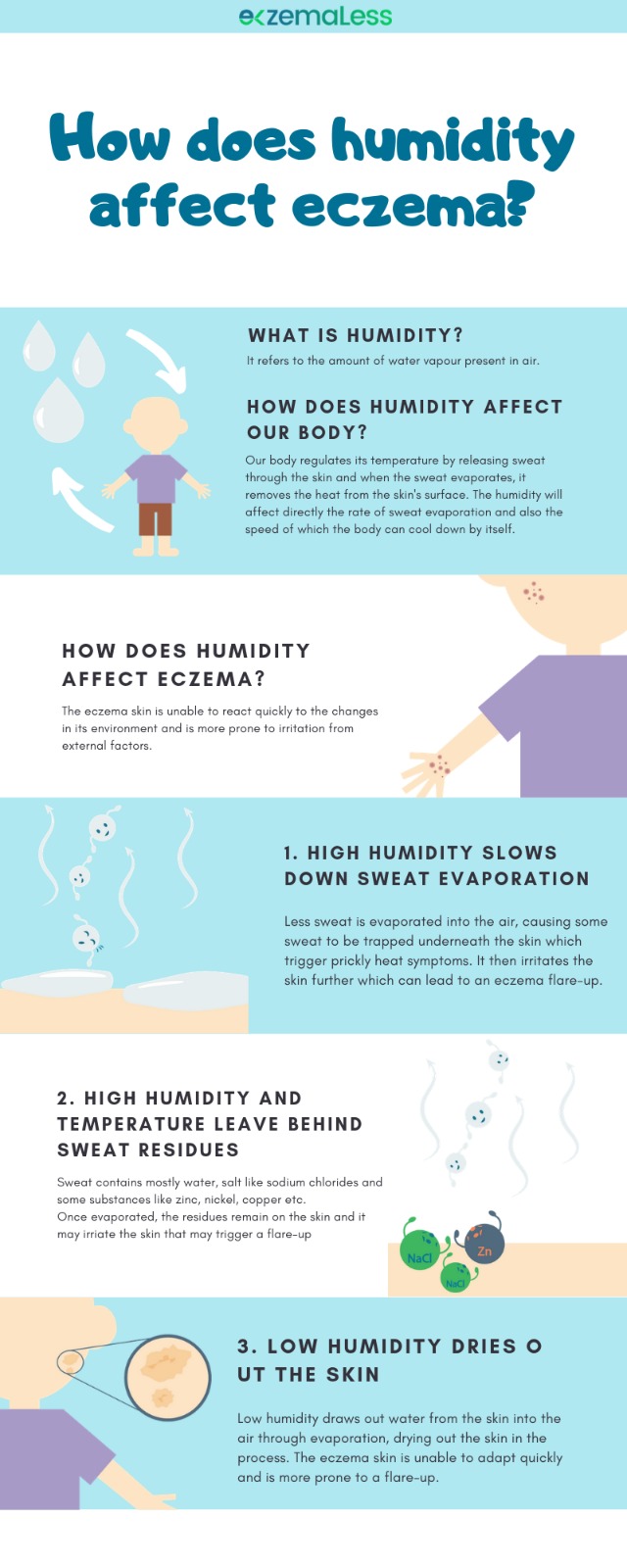
“What caused my Eczema to flare”, this is a question that bothers Eczema sufferers the most. It is very important for each individual to determine what causes their Eczema to flare or in other words what are the triggers that affect them the most. Usually, triggers are something that you encounter such as a certain type of clothing or something in the weather such as pollen or something that you have consumed. Triggers are not the same for every individual. Different triggers may cause a flare in different people. Some of the most common triggers are intense sweating, scratchy woolen clothes, pet dander, hot or cold weather, harsh soaps, and cleansers.
It’s very hard to say accurately what is the exact cause of eczema for an individual. Probably the genes play a vital role. If your parents are prone to Eczema flares, you may be, too. Another reason could be a weak immune system that fails to defend the body from attacks of external factors ultimately causing a flare. This is common for both Atopic Dermatitis and Contact Dermatitis wherein the former is more thought of chronic condition and the later though not chronic as Atopic Dermatitis but occurs only when your skin touches an irritant. Nevertheless, both types get flares from Eczema triggers.
Eczema Flares are common in babies and kids too. Eczema Flares are more troublesome at younger ages because babies have very sensitive skin and it is hard to prevent children from scratching themselves. Quite often children grow out of Eczema as they grow up. It is very well known that Eczema cannot be cured. However, Eczema can be managed by reducing the number and severity of Eczema flare-ups.
How to effectively manage Eczema Flare-ups?
As mentioned earlier it is very important to try to reduce Eczema flareups by knowing and avoiding your triggers.
Prevention Measures to avoid Eczema Flares
Avoid Irritants: There are certain products that cause Eczema flares when they touch your skin. These could be cleansers, perfumes, laundry detergents, soaps or food items. To know what product actually causes your Eczema to flare, you will have to track the products and do elimination trials which means that eliminate a product from your daily routine or diet for some time and see if that helps your Eczema. It is safer to switch to odorless and colorless soaps, cleansers, or laundry detergent.
Indoor Pollutants: Often tiny particles in the environment can cause your eczema to flare. Some of these are Dust, Cigarette Smoke, Pet Dander, Mould, etc. It is always good to maintain hygiene at home and work. Dust regularly, avoid pets if you are allergic to them, quit smoking or hanging out with those who do.
Clothing: One of the common triggers and perhaps the closest one that irritates your skin are your clothes. Avoid Scratchy woolen clothes, wear breathable fibers avoiding multiple layers or the heavy ones which make you sweat.
If your skin type is dry take extra efforts to keep it moist. Use body lotion soon after the bath, use moisturizer two or three times a day. Maintain a good humidity level in your bedroom while sleeping to keep the air moist. Drink plenty of water to keep your skin hydrated.
Winter: Dry air combined with indoor heating systems robs the moisture from skin making it dry and more prone to eczema flares. Use a thick moisturizer immediately after a shower to lock moisture in the skin, avoid hot baths and keep it short (use lukewarm water). Avoid rubbing your body with rough towels, pat dry instead. Use a humidifier to maintain the humidity level and curb dry heat pumped by the heating systems.
Treating Eczema Flares
Topical Steroids: Over the counter steroid creams are vital in reducing the red, itchy flares. If they don’t work you may need a stronger dose that can be availed with the help of a physician.
Moisturise: Keep your skin moisturized as much as you can. It softens your skin relieving pain and reducing the eczema flare especially if it is caused by dry skin. Have plenty of water and other liquids to keep your skin hydrated.
Take a Bath: A look warm bath may give you relief during flares. But remember, keep the bath short (not more than 10 mins). Apply moisturizer soon after your bath so as to seal the moisture of the skin and preventing it from drying.
Avoid Scratching: Scratching usually damages the skin, which can itself cause more flares to occur. Try to reduce scratching whenever possible. You could try gently rubbing your skin with your fingers instead. Keep your skin covered with light clothing to reduce damage from habitual scratching.
Wet Wraps: Designed for Eczema special medicated bandages, clothing or wet wraps can be used to cover the areas of flared skin. These bandages can be used over emollients or with topical corticosteroids to prevent scratching allowing the skin underneath to heal locking the skin moisture.
Antihistamines: If you have severe itching you can have a dose of Antihistamine as recommended by the physician especially during bedtime. Consider the side effects before consuming.
Care Plan: Maintain and follow a care plan created by either you or as recommended by your physician. It is very critical to take necessary action at the recommended time to overcome and manage flares effectively.
For timely recognition of flares and informed treatment decisions during clinic visits, guidelines advocate tracking of the disease by
a) monitoring possible triggers (e.g. allergens),
b) recording disease severity including specific symptoms and signs
c) response to therapy
Atopic dermatitis. The New England journal of medicine 2005; 352: 2314-24.
Manually maintaining detailed records of the triggers that you are being exposed to can be time-consuming. Also, it is important to record the regimen you are following and how well you are adhering to it. Traditionally people have maintained a paper diary to keep these records. Recently Health-Tech Companies have come up with Eczema Managing apps available that allow you to maintain digital records, tracking your regimens and triggers.
Visit a physician:
If your Flares don’t respond to your care plan, do not hesitate to visit your General physician. The Physician may recommend other topical or oral and may also recommend a referral to a dermatologist who can take a few tests and prescribe recommended medications.
GET IN CONTROL OF YOUR ECZEMA
Use our AI tool to check the severity of Eczema and keep track of your Eczema progress.