Impact of Varicose Eczema: Symptoms, Causes, and How to Find Relief
Varicose eczema, also known as stasis dermatitis, is a chronic skin condition often overlooked or misunderstood. This condition commonly affects individuals with chronic venous insufficiency, where poor blood circulation leads to skin changes and inflammation. In this article, we will delve deep into the hidden impact of varicose eczema, exploring its symptoms, underlying causes, and effective strategies for relief. Whether you are experiencing symptoms or seeking to understand this condition better, this guide will provide valuable insights to help you manage and treat varicose eczema effectively.
What is Varicose Eczema?
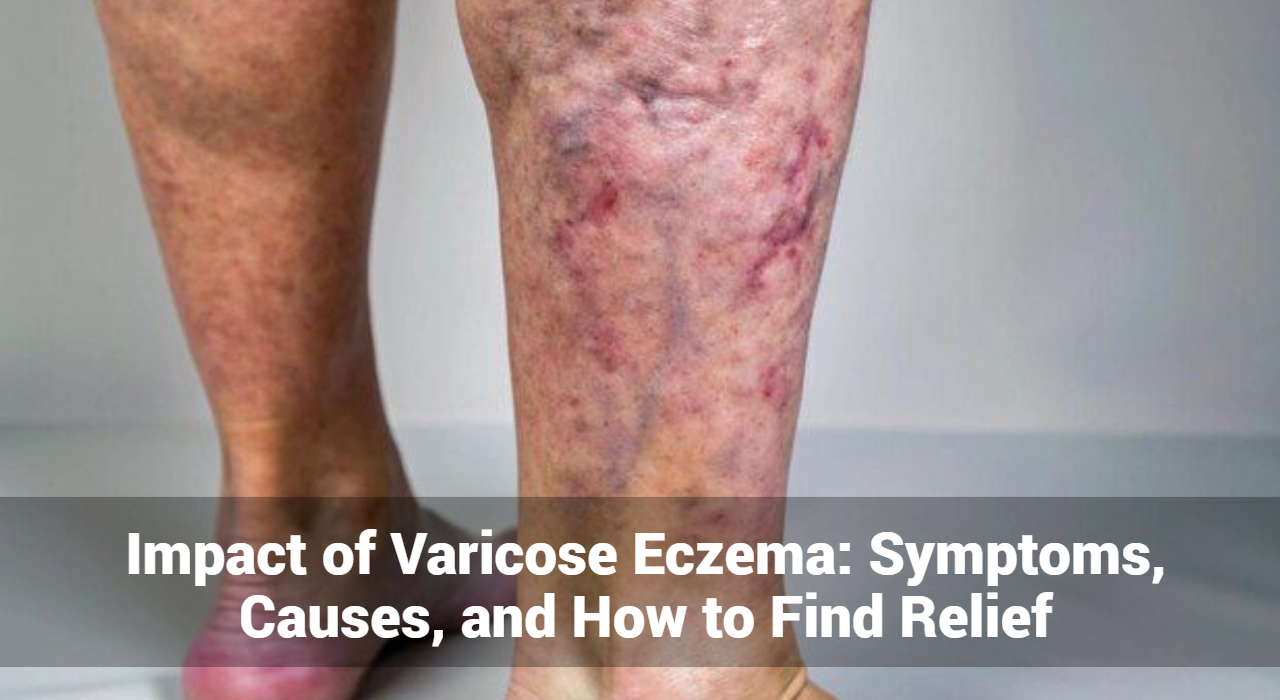
Varicose eczema is a type of dermatitis that develops in areas where blood circulation is impaired, typically around the lower legs. It is closely related to varicose veins, which are swollen, twisted veins that often appear on the legs due to increased pressure in the veins. The combination of poor blood flow and inflammation results in skin changes and symptoms that can significantly impact quality of life.
The Connection Between Varicose Veins and Eczema
The condition arises from chronic venous insufficiency, where blood pools in the veins rather than flowing back to the heart. This venous stasis leads to increased pressure in the blood vessels, causing leakage of blood components into surrounding tissues. Over time, this process results in skin inflammation and the development of eczema-like symptoms.
Track and Manage your Eczema treatment using a comprehensive Eczema App
Download Eczemaless now
What Are The Symptoms of Varicose Eczema?
Varicose eczema manifests in several distinctive ways. Here are the primary symptoms to be aware of:
1. Itching and Burning: One of the most common symptoms is intense itching and a burning sensation in the affected areas. The itchiness can become severe, leading to discomfort and an urge to scratch, which may exacerbate the condition.
2. Redness and Inflammation: The skin around the lower legs may appear red and inflamed. This redness is often accompanied by swelling and can vary in intensity.
3. Dry and Cracked Skin: Affected skin often becomes dry and flaky. In severe cases, it can crack, leading to pain and potential infection.
4. Brownish Discoloration: A characteristic sign of varicose eczema is the development of a brownish or purplish discoloration of the skin, known as hyperpigmentation. This occurs due to the deposition of hemosiderin, a byproduct of broken down red blood cells.
5. Ulcers and Sores: In advanced stages, varicose eczema can lead to the formation of venous ulcers or sores, particularly near the ankles. These ulcers can be difficult to heal and may require medical intervention.
What Causes of Varicose Eczema?
Understanding the underlying causes of varicose eczema is crucial for effective treatment and prevention. Here are the primary factors contributing to this condition:
1. Chronic Venous Insufficiency: The primary cause of varicose eczema is chronic venous insufficiency. When the veins in the legs cannot effectively return blood to the heart, pressure builds up in the veins, leading to blood leakage into surrounding tissues and causing skin changes.
2. Varicose Veins: Varicose veins are a direct contributor to varicose eczema. These swollen veins, often visible on the surface of the legs, signify poor blood circulation and increased pressure in the veins, setting the stage for eczema development.
3. Obesity: Excess body weight can exacerbate venous insufficiency by putting additional pressure on the veins. This increased pressure can worsen blood flow issues and contribute to the development of varicose eczema.
4. Age: The risk of developing varicose eczema increases with age. As individuals age, the veins may weaken, and the risk of chronic venous insufficiency and varicose veins grows.
5. Genetic Factors: A family history of varicose veins or chronic venous insufficiency can increase the likelihood of developing varicose eczema. Genetic predispositions play a role in vein health and skin susceptibility.
6. Sedentary Lifestyle: Prolonged periods of inactivity can impair blood circulation, leading to venous insufficiency. Sedentary behavior, such as sitting for long hours, can contribute to the development of varicose eczema.
GET IN CONTROL OF YOUR ECZEMA
Use our AI tool to check the severity of Eczema and keep track of your Eczema progress.
Diagnosis of Varicose Eczema
Accurate diagnosis is essential for effective management. The process typically involves:
1. Medical History and Physical Examination: A healthcare provider will review your medical history, including any symptoms of varicose veins or chronic venous insufficiency. A physical examination of the affected skin areas helps assess the severity of eczema and rule out other skin conditions.
2. Ultrasound Imaging: To evaluate the extent of venous insufficiency, an ultrasound scan may be performed. This non-invasive test visualizes blood flow and identifies any abnormalities in the veins.
3. Skin Biopsy: In some cases, a skin biopsy may be conducted to examine skin samples under a microscope. This can help differentiate varicose eczema from other skin disorders.
What Are The Treatment Options for Varicose Eczema?
Effective management of varicose eczema involves addressing both the symptoms and underlying causes. Here are some treatment options to consider:
1. Lifestyle Modifications
Making certain lifestyle changes can improve blood circulation and alleviate symptoms:
- Weight Management: Maintaining a healthy weight can reduce pressure on the veins and improve overall venous health.
- Regular Exercise: Engaging in activities such as walking or swimming can promote better blood flow and strengthen leg muscles.
- Elevating Legs: Elevating the legs above heart level when resting can help reduce swelling and improve circulation.
2. Compression Therapy
Wearing compression stockings helps manage symptoms by applying gentle pressure to the legs. This pressure supports venous return and reduces swelling, which can alleviate the symptoms of varicose eczema.
3. Topical Treatments
Applying topical treatments can provide symptomatic relief and improve skin health:
- Emollients: Moisturizers and emollients help soothe dry, itchy skin and prevent further irritation.
- Corticosteroids: Prescription corticosteroid creams or ointments can reduce inflammation and relieve itching. Use these products under medical supervision to avoid potential side effects.
4. Medical Interventions
In some cases, medical procedures may be necessary to address the underlying venous insufficiency:
- Sclerotherapy: This procedure involves injecting a solution into the affected veins, causing them to collapse and eventually fade.
- Endovenous Laser Therapy (EVLT): EVLT uses laser energy to close off malfunctioning veins, improving blood flow and reducing symptoms.
5. Wound Care
For individuals with venous ulcers or sores, proper wound care is essential. This may include cleaning the ulcers, applying dressings, and following medical advice for healing.
How Can I Prevent Varicose Eczema?
Preventing varicose eczema involves managing risk factors and taking proactive measures:
1. Stay Active: Incorporate regular physical activity into your routine to promote healthy circulation and prevent venous issues.
2. Maintain a Healthy Weight: Adopt a balanced diet and engage in regular exercise to manage weight and reduce pressure on the veins.
3. Avoid Prolonged Sitting or Standing: Take breaks to move around if your job or daily activities involve prolonged sitting or standing. This helps prevent blood pooling in the legs.
4. Use Compression Stockings: Consider wearing compression stockings if you are at risk for varicose veins or have a history of venous insufficiency.
Conclusion
Varicose eczema is a complex condition with significant impact on individuals’ lives. Understanding its symptoms, causes, and treatment options is crucial for managing the condition effectively. By adopting lifestyle changes, using appropriate treatments, and seeking medical advice, individuals can alleviate symptoms and improve their quality of life. If you suspect you have varicose eczema or are experiencing related symptoms, consult a healthcare provider for a thorough evaluation and personalized treatment plan.
Track and Manage your Eczema treatment using a comprehensive Eczema App
Download Eczemaless now



